The local health director is the chief health policy advisor to the elected officials in a jurisdiction for
- 1. Public health.
- 2. Assessment of Community Health Status
- 3. Access to Medical care.
- 4. Financing of health and medical care
He or she is responsible for short and long-range public health (including medical care planning) and for defining the department's vision (strategy) to meet public health needs for the community through using three principles or components:
- Assessment: (1)
- Goal and outcome definitions
- Financial analysis and budget development.
- Use of primary and secondary prevention.
- Use of environmental services.
- Access to medical care.
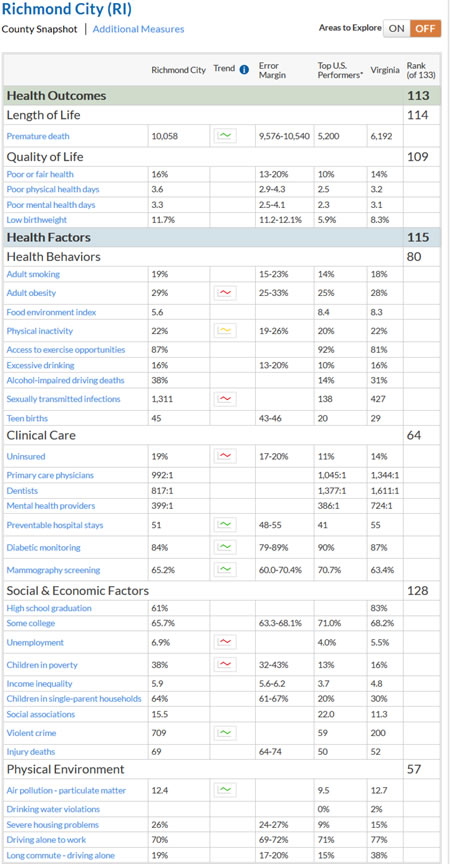
See Future of Public Health: A 1988 book published by the I.O.M. (Institute of Medicine, a branch of the National Academy of Sciences [NAS] defines the three components of public health. Read the summary, and scan book. Also, look at the 2003 updated version. Also look at the Health United States-2020. Finally review the RWJF Gaps in health status, Virginiain which allows you to compare data between states and between citizen counties. For example look at data for the city of Richmond for 2015: Go to site and look at other communities in the U.S. While this data is useful and comparable among many communities it needs to be linked to morbidity among specific common chronic diseases (Diabetes, CHD, Stroke, Arthritis, Asthma) not just morbidity for the entire constellation of diseases.
- Recommendations, and
- Assurance (accountability and quality control)
Each of these will be discussed in detail in appropriate essays in this series.
HEALTH DEPARTMENT PROGRAMS
Before examining the responsibilities and training incumbent upon a health director, a description of the scope of the health department in and outside the U.S. provides a base for comparison. The types of programs organized by a local health department depend on the region or country in which they are found. Programs may be unsophisticated if their purpose is simply to ensure that children are immunized, potable water is provided and waste is properly removed, as is typical of many developing countries. In most urban areas of the United States and Western Europe however, local health departments have divisions devoted to administration, technical support, environmental services, nursing, health education, and planning and clinical services. In addition to these typical public health programs, a department may also manage mental health and medical care services, as well as hospitals and nursing homes (Los Angeles & Chicago for example) . Finally, the department may also provide primary medical services to underserved populations. The detailed scope of these programs is discussed in chapters 7 through 9. The British NHS and The Canadian National Health System have spent considerable time and effort planning their programs, and ensuring universal access. The Virginia Department of Health’s website and visit the Strategic Plan which shows program responsibilities similar to those of the majority of the U.S. State Health Departments. In the last 2 years the National Association of City and County Health Officials has started local health department accreditation programs.
THE DIRECTOR'S RESPONSIBILITY
The local public health director should be able to manage either an unsophisticated health department in a developing country or a large urban health department in a developed country. Even in industrialized countries there are rural areas where health services are only marginally better than those in many developing countries (far southwest Virginia, rural Kentucky). The health director, the community's health advocate, is responsible for developing grass-roots support for many kinds of health services. Private and public efforts should be blended to meet defined goals and objectives. Every health department needs to develop special-interest support groups, such as local boards of health to promote policies throughout the community. Special emphasis should be placed on educating elected public officials to whom roads, schools, water, and sewage may be the most visible and expensive parts of the public infrastructure.
A health director needs the support of elected officials to develop the department's programs while working with the private health care sector to integrate public health programs into the community's total health care system. Both politicians and the private medical sector educating about their joint responsibility to help plan and manage the manpower, capital, and services that make up the complex health care environment, of which public health is just a part.
DIRECTOR'S TRAINING
Although many public health directors in the United States are physicians, some communities choose health care administrators or other public health professionals (nurses and health educators) as directors, especially since both trained/certified public health and primary-care physicians are in short supply. Public health physicians often begin their careers in a primary care clinical setting, then become assistant health directors in large departments, or enter preventive medicine residencies. Medical schools that have public health and preventive medicine residents ensure their residents develop their clinical and epidemiologic skills.
It is advantageous for a preventive medicine specialist to be trained as a generalist (primary care) first. Having several years' practice, as a generalist, enhances understanding of how the skills of population medicine mesh with the skills needed for clinical care of individuals. This improves communication with the private practice medical community allowing the public health director to demonstrate an understanding of clinician’s problems. The clinical skills of the primary care physician, particularly experience in treating chronic diseases (currently an increasing epidemic in the USA) relating to behavior, are valuable when talking to other members of the patient care segment of the community. By contrast, public health residents trained immediately after completing their MD rarely encounter the clinical or private practice problems seen in primary care medicine. Since 1990 it has become more common to find physicians who have completed a residency in primary care, followed by primary care practice and then a residency in preventive medicine. Additionally, more of these physicians are supplementing their medical training with degrees in law and/or public administration. Nevertheless, only a minority of local health directors have such training. In small communities with limited populations (less than 75,000 people), Nurses may serve well as local health directors, as they, like physicians, can speak from a biological understanding with community physicians.
The health director who comes from a background other than medicine (particularly health administration) will find it advantageous to have spent time in a clinical setting, to be able to relate to issues of access and cost of health services as well as understanding how population based services can improve health status.
Just as training requirements have increased in other fields, they are expanding in public health. The residency in preventive medicine requires a minimum of a year in a ‘transitional’ internship followed by a master's degree in public health including specialized training in public health program administration; environmental health, biostatistics, and epidemiology (see the requirements of the Residency Review Committee (RRC) of the Accreditation Council for Graduate Medical Education (ACGME). This is usually a 10 to 12-month course for a physician, followed by a year of practical training to ensure that the skills taught in the Masters of Public Health course (MPH course) are demonstrated in practice. Further emphasis has been placed on such training by the 2007 report of the Institute of Medicine (IOM). For non-physicians the MPH program is likely to last 2 years. Skills needed by public health practitioners have also multiplied. Increasingly training includes courses in genetics, toxicology, mutagenicity, teratogenicity, hydrology, waste management, maternal health, behavioral science, information systems and hazard assessment. Comprehensive curricula that include these topics are being developed in schools of public health and medicine throughout the United States. Deficiencies seen in the application of clinical preventive interventions, seen among physicians completing primary care residencies, or direct from private practice, show that the curricula in both medical and public health schools need updating. MPH courses are accredited by the Council on Education for Public Health (CEPH.) In the future more health directors will come from people with backgrounds in health administration, nursing, behavioral science and environmental health as the focus of public health shifts from prevention of infections to control of chronic diseases. In 2008 a Certification in Public Health became available for the first time for Non-MDs, or MDs without residency training, to attest to their competence in basic public health skills. This is offered by the National Board of Public Health Examiners. Concurrently the National Association of City & County Health directors, and others, have developed certification standards for local health department agencies.
THE DIRECTOR'S SUPERVISOR
Usually, though not always, a health director has two or more masters. Many local health departments serve multiple jurisdictions, including combinations of cities, towns, and counties in which there may be disagreement among the elected officials about priorities for funding and service. The health director may report to a non-physician city manager and a county executive. In some states, they report to a state health commissioner as well, through a regional public health system. Only health directors in the larger counties and cities report to a single supervisor.
COMMUNITY HEALTH CARE PROBLEMS AND MEDICAL CURRICULUM
In 1961, Kerr White(3) described the medical problems likely to affect a random sample of 1,000 Americans in any month. Of particular interest, was the finding that for each sample of 1,000 adults that had an episode of illness, consulted a physician, were hospitalized, and needed consultation, only one needed referral to a tertiary care center.
This study was updated in mid-2001 with similar findings, as shown above. Unfortunately, medical school curricula are still focused on treating the one in 1000 referred to the medical school (although this is starting to change), not the other 999. In the 1960s and 1970s, Maurice Wood, in the department of family medicine at the Medical College of Virginia analyzed the types of medical problems occurring in primary care and confirmed Kerr White's original studies. Additionally, data from the 1978 National Ambulatory Care Survey (NAMCS) showed that of over 760 conditions reported by primary care physicians, were responsible for the problems seen in their practice, and 155 were responsible for 95% (CMGB at Eastern Virginia Medical School: 1978 -1980). More recent studies from the NAMCS surveys confirm that primary care content changed very little. Ten conditions, of which pregnancy and heart problems are the most common, lead to the majority of all admissions to all hospitals, not just community hospitals. As medical schools become more attuned to the market need for care seen by their graduates, as opposed to the conditions about which tertiary-care specialists (the majority of clinical teachers in medical schools) teach, many are changing their curricula to one closer to that taught in most other developed countries. Medical schools in other countries focus on producing generalists who provide the majority of care. This change has been stimulated in the US by a Robert Wood Johnson Foundation program, The “Generalist Initiative.” But unfortunately most medical schools have only given lip service to the project. The new Affordable Care Act contained within its multiple objectives some that could lead a greater proportion of primary care physicians although funding to enhance such programs in medical schools remains missing and residency training positions are not increasing.
PHYSICIAN OR NON-PHYSICIAN DIRECTOR?
Because most physicians lack administrative skills, particularly in budgeting, accountability and financial management, some states and local communities select non-physicians as health directors. They may be trained as health care and nursing administrators in schools of health administration, hospital administration, or even public administration. The ideal background is a combination of patient care and organizational management skills. The master's degree in public health alone does not adequately prepare either a physician or non-physician for administrative duties. It deals mainly with technical public health issues. Training for health care administration is very limited in programs for public health, despite the existence of departments of health administration in many of these institutions. It teaches administration of 'normal' programs in such fields as maternal and child health, infectious diseases, and environmental medicine. For public administration skills, one needs a degree in public administration at a school of business or health care administration. Physicians and nurses in the military services who specialize in preventive medicine and public health have a number of educational opportunities available in general and medical administration (school of hospital administration, command and general staff college, the industrial college, and the three services’ War Colleges). These courses are also available, at no charge, to military reservists They offer preparation in health care administration in the public health sector as well as the military. With the current military interest in civilian support programs Afghanistan and Iraq) these skills are needed more than ever.
NON-MEDICAL SKILLS NEEDED
Public health directors need skills in negotiation, leadership, persuasion, clarity in written and verbal communication, technology and data collection and management, and effective public presentations of issues. They must develop interpersonal skills that promote open discussion of complex and often highly volatile issues. Expertise in financial analysis is essential to explain budget priorities to the agencies that fund local health department programs. The ability to use a computer and communicate electronically is essential today. Personnel evaluation skills are necessary to find and retain high-quality staff. Leadership is a skill that may be taught in Medical schools In the past they taught physicians to work in the individual entrepreneurial environment, but are starting to teach team practice where the physician is a leader for the whole team. Past experience with physicians, unable to adjust to working as a team member, has been another reason many communities choose non-physicians as health directors.
LEADERSHIP
Leadership ability lends credibility to both the individual and to the department he or she represents. It involves a willingness to listen to others' views, to not take sides until all issues and their ramifications have been presented. It also involves a willingness to take advice from many sources, to be a team member, and to allow others to lead the team when necessary. It is important for directors to accept all individuals based on performance, without regard to sex, race, age, or religion. Leaders have attitudes that encourage people to work with the health department. If the directors are physicians, they don't allow their professional accomplishments to deter people educated in other disciplines from presenting their own views as community leaders. Leaders also develop many advisory groups, including both professionals and consumers, to work with the health department.
CREDIBILITY
As a public health specialist (lay or medical), you have the opportunity to improve the health of thousands of people. Your ability to make such impact depends largely on your personal credibility. A health director is in the public eye all the time. Consequently, to move programs forward, you must be perceived as a caring, innovative, resourceful leader.
CONSULTANTS
Non-physician health directors need consultants to advise them when biological issues must be resolved. These consultants may include practicing physicians from local medical institutions and from schools of medicine, dentistry, and allied health sciences; nurses, pharmacists, hospital and nursing home administrators. Executive staffs of the health care associations may also serve as consultants. Without this backup, it is difficult for non-physician health directors to speak credibly about medical issues such as infant deaths, premature births, immunization standards, primary care, environmental health, toxicology, health hazard appraisal, and genetics.
READINGS:
- Future of Public Health IOM – 1988 p7-8
- Essentials of Public Health, Turnock 3rd edition
- K. L. White: “The Epidemiology of Medical Care,” N. Engl. J. Med. 263: 885-892, 1961
REFERENCES:
- Reigelman R K: Studying a Study and Testing a Test (Boston: Little, Brown), 1981.
- Swinscow T D V, ed: Statistics at Square One (London: British Medical Association), 1978.
- Buttery C.M.G: The Health Directors Handbook. Oxford University Press. New York, 1990
- Introduction to Public Health, 4th Edn - Schneider, MJ. 2013
- Essentials of Public Health Management. Fallon LF & Zgodzinski EJ, 3rd Ed: 2012;
- Governing by Network. 2004, Goldsmith & Eggers
- The Future of Public Health in the 21st Century (Washington DC, IOM, 2003)
Links to Health Policy Groups:
The Robert Wood Johnson Foundation
The Commonwealth Fund
The Kaiser Family Foundation
The King’s Fund