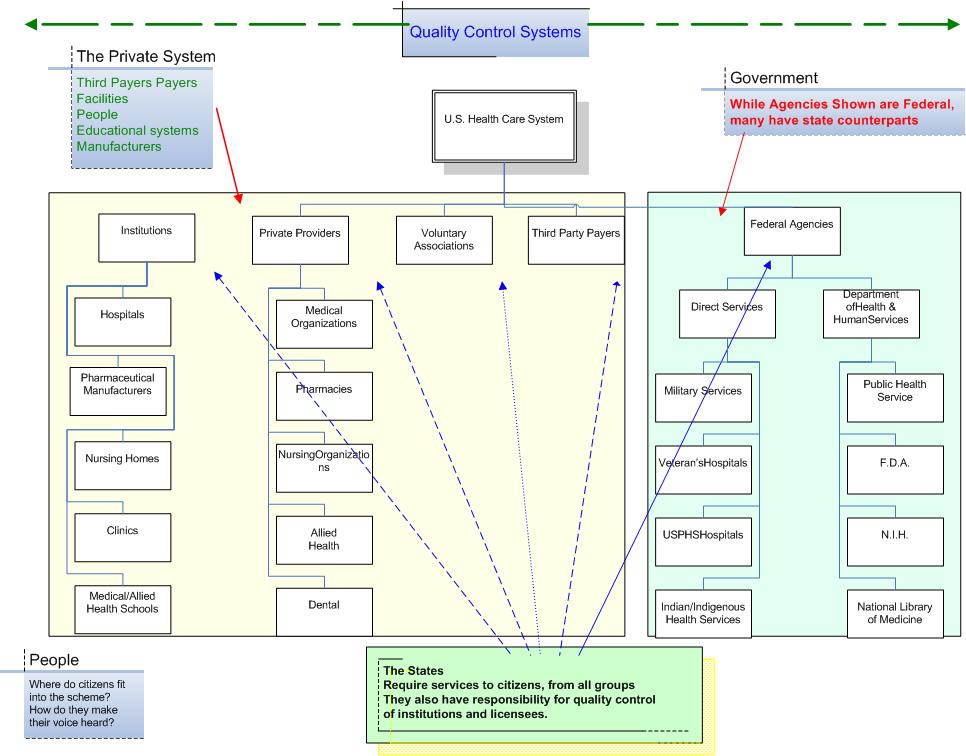
| The ‘health care’ system includes ALL the elements of the health and medical care systems found in the federal, & various state governments, and developed by all the independent private entrepreneurs. For the purpose of this discussion those organizations that are not part of an organized government entity (even though they receive much funding from government agencies, such as hospitals) are placed in the private sector. While this system has been described in many books these descriptions are always several years behind reality and tend to focus on the organization as seen by interests other than public health. The ‘view’ in this case is framed more as descriptive epidemiology. What is it? Where is it? At what time is it? How has it reached its current form? What are its current attributes? |
| This consists of institutional members such as hospitals and nursing homes, and groups of people organized for the most part by their specialized training. |
| The institution's major cost center is the hospitals. They consist of private freestanding hospitals such as the Health Corporation of America facilities (HCA). This is just one group of the more than 6000 currently licensed hospitals. Many of these hospitals, like those in Virginia, only use 50% of the total number of beds that they are licensed to provide. Attempts to consolidate hospitals to make them more efficient have, for the most part, been fruitless. While the HCA group is a strictly for profit group, many other hospital groups are organized as “not for profit” (NFP). The VCU University Health System is a typical Non Profit organization. Most Hospitals in the U.S. are free standing, mostly not for profit, originally organized as community service organizations. Many of these were developed in health care shortage areas after WWII, with the expectation that they would bring doctors, nurses and other services into these mostly rural areas. They were developed with funding from the Hill-Burton program. This program required that any facility developed with its funds had to dedicate a significant proportion (although not stated) of its services to the poor. Other than a requirement for service to the poor there were no quality standards attached to this program. Among these Hospitals we also find the nations 125 Academic Medical centers including the medical schools who while members of the American Hospital Association (AHA), are also members of another special interest group the AAMC, Association of American Medical Colleges, which sets standards for training at pre & post MD level as well as lobbying congress for continued support. |
| The Pharmaceutical and medical implement manufacturers. These are many and varied as can be seen at the Pharmaceutical Related Organizations, Associations web list. Among these are world giants such as Merck, Squibb, Burroughs Welcome and others represented by the Pharmaceutical Manufacturers Association (PhRMA). These manufactures and researchers are currently at the center of debate about the cost of drugs used in particular by the chronically ill and the aged. Prescription costs are a major debate in Congress and state governments at present. |
Another
group of institutions responsible for a large
share of medical expenses is the nursing home group
represented by the American Health Care Association
(AHCA),
which represents almost 12,000 nursing facilities
with more than 1.5 million beds. A bed day in a typical
nursing home in Virginia
is reimbursed about $80/day for Medicaid patients. Think
bout this in terms of 365 days a year for the 1.5
million beds. This does not include the costs
of private beds in many institutions which may be
well over $150.day, but still far less than a hospital
bed which in Virginia is about $375/day. IN
addition top the free standing nursing homes some
hospitals have areas designated for sub acute
(nursing home) care, while many Community centers
for older citizens have sub acute beds for their
own members.
|
| Among Hospitals we also find the nations 125 Academic Medical centers including the medical schools who while members of the American Hospital Association (AHA), are also members of another special interest group the AAMC, Association of American Medical Colleges, which sets standards for training at pre & post MD level as well as lobbying congress for continued support. |
The various medical professions are found among the physician, allopathic. osteopathic and homeopathic who are trained in colleges of medicine accredited by the AAMC. While 50 years ago the branches of training were divergent, they are similar today. State Boards of Medicine license them by common examination. It is among the specialty (trade) groups that there is discrimination. For example an osteopathic physicians, completing a residency in preventive medicine will not be licensed by the American College of Preventive Medicine even though their skills cannot be differentiated from those who trained at a non-osteopathic medical school. This is due to the current specialty trade group, the ACGME (Accreditation Council for Graduate Medical Education), which control training and activities of he various residency standards groups (Residency Review Committees.) The encompassing trade group for physicians is the American Medical Association. However, less than 50% of physicians belong to the AMA. Subsidiary to the AMA are all medical specialty groups, about 200 at present. The graduate accrediting committees include 27 residency review (click on the residency review committee link) committees, although some of these committees have a number of subspecialty reference groups. For example, Preventive medicine includes general preventive medicine, public health, aerospace medicine and occupational medicine. Physicians, taken as a whole, fall out as two major subgroups; primary care physicians and specialty physicians. In all countries except the U.S. medical schools train their students to be primary care physicians. Selection for specialty training is not usually made until the newly graduated physician has started his or her first postgraduate year, called an internship in the U.S. and a “junior house staff” position elsewhere. The primary care physician, labeled a general practitioner in other countries, but a family physician, general pediatrician or general internist in the U.S. is expected to be the entry point into the medical are system. The primary care physicians (see the AAFP definition) should be able to care for 90% of he problems coming into their practice, they should be accessible either directly or through an associate 24/7, they should provide continuity of care at a reasonable fee. They should guide their patients to appropriate specialty care when indicated. Compared to all other counties we have a surfeit of physicians performing many procedures, not because of clinical indication but for legal protection. |
| Pharmacists may practice in hospitals, group practices, where allowed by state law, in community pharmacies, or in the pharmaceutical research industry or the federal government. Their trade group is the American Pharmacists Association (APA) but just like physicians there is a myriad of other specialized trade groups depending on their employment site. The majority of pharmacists, like physicians, practice in the private sector. |
| Nurses comprise a wide range of skills from the licensed practical nurse ( 1 year of training) to an associate degree nurse ( 2 years at a community college) to a three year diploma nurse and a four year college degree nurse. The last three, despite their different lengths of training all take the same examination to work as a nurse! Then there nurse specialists who train as nurse practitioners to extend the scope of a medical practice by managing the more routine and chronic disease problems, allowing the physicians to exercise their greater diagnostic skills. Nurses by tradition, except for public health nurses, have worked mostly in hospitals. A medical science develops new treatments more patients are treated in ambulatory settings outside hospitals and hospitals are becoming centers for the critically ill cared for in Intensive care units nurses are specializing more in critical care skills or moving to the ambulatory settings. Just as for physicians there is a single nationwide organization, the American Nursing Association (ANA) serves that purpose for nurses. There are also specialty nursing organizations just as for medicine, as well as statewide and community based organizations. Every place there is a medical/health care institution there will be nurses. |
| There are a myriad of allied health organizations. The allied health term coves all the health related professions except dentists, physicians and nurses. This includes physical and occupational therapists, audiologist, dieticians. counselors, laboratory technicians, radiology technicians, emergency medical technicians (of all types), and health care administrators at a minimum. Each has their own professional trade association. Each is in competition with doctors and nurses to be labeled individual practitioners so they can bill third party insurers for a piece on the medical money pie. |
| Dentists are probably the last of the individual medical entrepreneurs. Most dentists still work as practitioners with their own practices or in small groups. A few work with group practices such as the Kaiser Permanent group, or in the HRSA supported community health centers. They also have generalists and specialists, found mainly in urban centers With the improvement in diet and application of fluoridation the need for dentists has declined somewhat, and at least two dental schools have closed in the last 10 years. The dental trade group is the American Dental Association (ADA) which advocates for dentists just as the AMA advocates for physicians. They also have state and local organizations and specialty organizations just as doctors and nurses do. The main difference between dentists and doctors is the failure of many third party insurers to cover dentistry. |
While not limited to health care, voluntary organizations play a large role in thos arena. While the professional organizations echo the needs of their members the voluntary organizations, for the most part act on behalf of patients or potential patients. Every disease and organ system has an organization. For example the American Lung Association started in 1904 to fight Tuberculosis changed its focus in the 1970’s when Tuberculosis appeared to be controlled to focus on other diseases of the respiratory system such as cystic fibrosis, chronic obstructive disease, and cigarette smoke, even though these diseases already had activist groups. Just like the AMA the Lung Association has state and regional branches. The American Heart Association, another organ based group. This one focuses on the entire cardiovascular system and works with stroke victims and hypertensive patients as well as heart disease problems. Some of the associations have developed from older organizations when medical science reduced the need for them A major example is the Polio Foundation which was loosing members after Jonas Salk develop the vaccine. It turned its focus on children becoming the March of Dimes organization focusing on birth defects. The voluntary organizations have fueled major research with funding from donors as well as by pressure on Congress. One of the most successful of these has been the American Cancer Society. Not only has this association funded research but has acted as an information resource for patients and relatives of those with cancer. It has assisted regulatory agencies and quality control organizations in development of standards for care. Among the semi-official and voluntary organizations in the private sector are a multitude of foundations that focus on health problems that can be solved by population approaches to research.. The premier of these is probably the Robert Wood Johnson Foundation formed in 1972 by the board chair of the Johnson and Johnson Company. This foundation focuses on Access to Care, Chronic health conditions, healthy communities and harm caused by substance abuse. We have had three recent grants in Richmond from the RWJF. One managed by Dr, Buttery, One by Dr. Lanier and one jointly. Another m ore recent foundation that has given big bucks for research and application in health care is the William and Melissa Gates Foundation. This foundation has funded development of a Malaria research center at Hopkins School of Public Health. It has funded a global AIDs/Tuberculosis program with more money than entire nations are giving to the cause. Like the RWJF it has also provided a focus on worldwide immunization against childhood diseases. |
If the patient is the first party to the health care contract, and the doctor the second, the entity that pays for the care is the third party. For most of us, this third party is one of the multitudes of insurance companies that either cover individuals (this coverage has become too expensive for the vast majority of families or individuals) or cover employees, which is how most of us get our coverage. Government as a third party will be covered in the section on the federal sector. Until the 1930s health insurance was unknown in the United States, until Blue Cross-Blue Shield was founded.
With the merger of the American Association of Health Plans (AAPH) and the Health Insurance Association of America (HIAA) approved on October 21 of 2003 this joint conglomeration, representing some 200+ insurance companies, covers 200+ million people or 66% of the population. Many of the remaining insured are covered by federal personnel system plans including the uniformed services plans. This still leaves some 47+ million currently people uncovered by any form of health insurance. This topic will be covered by Dr, Lanier in his discussion of health care reform. We can only hope that with this umbrella of the vast majority of third party payers that a common application form, a common medical reimbursement form, a commitment to preservation of health rather than treatment of disease might be forthcoming, although I would not hold my breath. |
| The Military (Uniformed Services) which a continually reorganizing its care into two sectors, that for currently serving members and their families and retirees. Family members who are not in the services are covered by contracts with third parties. It is basically a self insured program that gives relatively free choice to those enrolled unless they live in an area served by an HMO such as Kaiser Permanente. Retirees have the option of care in the private sector or at military hospitals, unless they are eligible for the Veteran’s Administration program. Care in military hospitals in increasingly being restricted to military members with dependents being seconded to the Private sector. The major difference is that coverage under the military health systems is more comprehensive than most civilian insurance program. While there are a few free standing military hospitals such as Walter Reed Army Hospital and Bethesda Naval Hospital most military hospitals are located on active duty campuses where their main focus is on maintaining the health of military members. The care provided in the military is a model for civilian occupational medial programs. The military system has a uniform medical data set for each member, but most of these are still in paper form and are carried around with military members and subject to all the problems of a paper base d system. Military members however have a system that is more akin to a socialized (a centralized) system and just like members of the UK system would like to see improvements but do not want to do away with it |
| Care of military veterans who are injured on duty, or develop diseases that arise from their military duties are provided long term medical care after discharge from the military by the Veterans’ Administration Health System. The VA keeps an interactive map of its health care facilities showing the 152 sites now available. The care at Veteran’s hospitals is as good as the care at any teaching hospital in the private sector. The V.A. is the singe largest source of medical residency training in the U.S.. If focuses on care of chronically disabled veterans who need both comprehensive and continuous care. |
| The U.S. Public Health Services started out as quarantine centers for seaman and were located in seaports. Over time this member of the uniformed services provided health care to the US Coast Guard they added additional duties such as providing hospital for all seamen in the merchant marine, for native Americans and staffed the Health Resources Services Administration with its initial emphasis on maternal health acre, then expanded into community health centers, training of residents and staffing of the clinical components of the Centers for Disease Control and Prevention. |
| Native Americans are provided health services through the DHHS’ Indian Health Services for American Indians and Alaska Natives, the details of which can be found at on the Medical & Professional programs we site. The majority of the staff providing health care are Uniformed Public Health Services Professionals. The care is provided through clinics on the Indian reservations and at the Public Health Hospitals. |
The constellation of non-service federal health programs are found within the Department of Health & Human Services (DHHS).> The programs consist of payment of medical services acting through two “third party” programs that started in 1965, Medicaid and Medicare. You will learn more about these programs as the course progresses as well as in HAD 692 and Dr Lanier’s course on health policy. |
| DHHS, through its pubic health services also supports the Centers for Disease Control, The National Institutes of Health, and the National Library of Medicine. We will be discussing and visiting all these sites during the course. |
| DHHS also exerts quality control over drugs and food through the FDA. |
| DHHS, through its pubic health services also supports the Centers for Disease Control, The National Institutes of Health, and the National Library of Medicine. We will be discussing and visiting all these sites during the course. |
| As part of the NIH serves as the medical library for DHHS & all its agencies |
| The States focus on their own populations and for the most part manage a subset of the DHHS programs. They are a 50/50 partner with DHHS for Medicaid. Many public health department, state and local, have staff members seconded to them from the CDC for various programs. State and local health departments apply to HRSA for grants in aid to develop community health centers and maternal health programs. The Medical Schools in the states obtain funding from the NIH, work in tandem with nearby VA hospitals and are starting to work with the federal agencies to assure quality services through its role in supporting Residency Training programs in medical schools and teaching hospitals The states complain, with justification that the federal government imposes national programs and costs, without consultation and enforce standards without consideration of the different populations and environments within the separate states. In what should be one of the advantages of states is that they, not the federal government, license the heath care professionals and the health care institutions. Almost without exception the states fail to perform long range health care planning, except in the few states that retain Certificate of Public Need Programs, such as Virginia. The original intent of this program was to license (and thus allow development of) new facilities and programs for health care. While fine in theory they have done little more than keep the state hospital associations happy by preventing new groups or programs from entering the state, thus reducing competition and innovation. |
People/Residents/Citizens. By whatever name, these are supposed to be the happy recipients of all the forgoing largesse. They have been treated by all and sundry in a patronizing manner for the last 200+ years. People as consumers are starting to demand a voice in development and access to services. As more people are disenfranchised by the increasing cost of care they are pushing for a national health system. 50 years ago when I started practice I charge $3.00 for an office visit. I only needed an office nurse and a part time secretary. I collected BX-BS reimbursement for surgical services and some hospitalization. When I decided to move to preventive medicine Medicare and Medicaid had just been developed and paper work was starting to increase. Law suits were rare. Since then many procedures are previously performed by primary care physicians are now performed by specialists as a counter to ill considered lawsuits decided by ill informed juries and judges. Concern about medical costs, and poor interpersonal relationships with many in the health care field have soured many people about the future of medical care. They do not now who to turn to about the issue of quality which has often been blown out of proportion by poorly researched new stories. One of the best examples is that of people refusing immunizations for themselves and their children because of unfounded stories about the dangers of immunization. |
| Having
looked at the base of care, people, we need to look at
major overarching issue of care - quality. The health professions have been interested
in quality control for thousands of years. In Ancient
Egypt a physician could use a trephine on a patient with
the understanding that if the patient died, so would
the physician. This gave meaning to the phrase “First,
do no harm”. Since Flexner’s developed the John’s Hopkins Model of medical care and training early in the twentieth century, death conferences have been used at teaching hospitals to learn whether anything the medical staff did contributed to the death, or whether something unforeseen occurred that could be prevented in the future. For some 30 years unexpected deaths have increasingly resulted in lawsuits which have resulted in an increasing vigilance because of the cost of defending against such suits, even in no guilt was found. In September of 1999 the Institute of Medicine (IOM) published “To Err is Human: Building a Safer Health System.” This work suggested that many errors could be avoided by improving the infrastructure of data collection, dissemination and performing better coordination of care. This was followed by another text in 2001, at the end of the third phase of work to improve care “Crossing the Quality Chasm: A New Health System for the 21st Century”. This work was based on changes to the delivery of care process, not on changing the way to pay for care. How is quality measured and who is responsible? This will be a topic in the future but the players include patients who must let health professionals know about adverse effects without running to lawyers. Hospitals and ambulatory care centers must have active quality review committees who look at all adverse outcomes (see JCAHO). Finding adverse outcomes requires both a good database on outcome, as well as an environment to examine the outcome without rushing to lay blame. Licensed professional must have their own review committees within their peer groups, as well as at the licensing committee level. The rush to put all adverse data on the ‘web’ may do more harm than good. Individual providers must have better data system than 3x5 cards with scrawled notes. Electronic patient databases are starting to permeate doctor’s offices (see AAFP). They have a long way to go in content, reliability and validity. JCAHO focuses in facility and program standards for hospitals, nursing homes, ambulatory care centers among others and has a contract with DHHS to review these facilities when they care for either Medicaid or Medicare financed patients. This means that virtually all health care facilities are covered. The individual professionals are licensed within each state. The licensing boards have a responsibility for quality, but are hampered by lack of data, except for the most egregious cases. Their operation in the public eye detracts from their ability to act as educators rather than adversarial police. They are responsible for ensuring that physicians out of medical school have met minimal educational standards including the United States Medical License Examination (USMLE). The Virginia Board of Medicine (VBM) functions at the state level as an arm of the national federation of state boards. Similar boards also license nurses, dentists, pharmacist and the allied health professional members. Other than physicians and dentists in private practice the other professionals work for an entity that has responsibility for their performance and discipline. At the National level, the professional associations such as the AMA recommend standards and advise regulatory agencies and elected officials on legislation needed to ensure them, through collaborative groups such as the NPSF – The National Patient Safety Foundation developed in response to the IOM study “To Err is Human”. At the national level the Institute of Medicine (IOM) continues to study the infrastructure of medical care to examine the role people and technology play in causing and preventing errors in medical care. Further, The Agency for Health Research and Quality (AHRQ) provides evidence based standards for care by assessing technology and reviewing research. Along with national organizations such as the Heart Association and Diabetes Association, it recommends standards of care within medical institutions and practices. There is a quality review board or committee in institutions reviewed by JAHCO. Their work is reviewed during JACHO inspections for compliance with the various clinical standards. On Dec 3, 2003 JCAHO announced a Universal Protocol to prevent injury during surgery, This will be placed into effect for reviews conducted after June 2004.There are no inspections of clinical ambulatory practice practices. AHRQ also recommends preventive interventions and sets guideline standards through the United States Preventive Service Task Forces (USPSTF) which are usually adopted by professional associations first, then by individual practitioners. AHRQ also reviews recommendations by national specialty groups and publishes guidelines through the National Guidelines Clearing House (NGC). Quality of Pharmaceutical preparations and medical devices is the responsibility of the FDA. One of the few remaining areas with no quality control is that of “herbal’ remedies and other alternative forms of health care. The NIH has been tasked with developing a study group on alternative remedies. The majority of knowledge of effectiveness is currently based on anecdotes. not on controlled research. The little that has been performed has been unable to demonstrate consistent effectiveness. Despite such evidence billins of dollars are spent on alternate forms of care annually. Remember that quality covers many parameters such as: Effectiveness, Benefit/harm evidence, Efficiency, Cost effectiveness, Replication Part of the problem I getting standards adopted is that there is no law that requires it. Practitioners tend to adopt them if they see that following the guidelines will keep them from being sued successfully, or if the guideline will improve their income. The latter occurs when the third party payers agree with the guidelines and adopt them as a prerequisite to payment. This complex issue is still evolving rapidly and the IOM is looking at ways in which technology can reduce errors through data based algorithms to detect deviation from the norm. |
| Ambulatory
care is provided by physicians in their offices
(known as clinics on some states), This care is also
provided a ‘clinics’ for the [poor associated
with teaching hospitals. Although much of this care is now being melded into the private (paying patient) programs so there is no longer a group of ‘poor’ patients used as subjects for training medical students. The ambulatory clinics also include surgical daycare centers developed by surgical specialists who found their income was improved by developing free standing units not associated with hospitals. Further they were not bound by hospital standards or by surgical suite rotation where senior surgeons had access priority. Free standing radiological centers have also been developed for the same reason. Although most states have licensing authority and have tried to limit the ambulatory day center proliferation such efforts have been thwarted by a combination of court decisions on legislative actions carried out at the request of professional organizations. Ambulatory care institutions have been enhanced by groups such a Kaiser Permanente which link ambulatory care to hospitals and nursing homes to provide regional systems which cover the gamut of services and try to keep an individual, once captured, within the system for all types of care. Other clinics have been developed in underserved areas of the country, both central city and rural, through activities of the Health Resources and Services Administration’s Bureau of Primary Health Care. This bureau funds community health centers with 100% start up funds slowly decreasing to usually less than 30% once established (normal 4-5 years). These centers must be open to all citizens, although they have a commitment to poor persons. They must have a board of directors selected from their clients. In addition to these clinics the bureau also has started providing support funds to look alike clinics, which serve similar populations in similar areas and ate having difficulty surviving due to service to many patients unable to pay for care. A local example is the Hayes Willis Health Center in South Richmond. Further, started in Virginia in 1991 by the Virginia Health Care Foundation, and now being copied in other states, is a coalition of Free Clinics. The free clinics started out as a number of small one night a week programs, usually rural, conducted by volunteer health care people. Over the years it has expanded, in many cases, to five days a week providing continuity, not just episodic emergency care. |