Under the general rubric of promoting and protecting the public's health, the health director and staff face a daunting array of programs designed to preserve and promote public health, from licensing septic tanks, monitoring the quality of air and water and minimizing accidents to conducting campaigns aimed at reducing blood pressure, intake of alcohol and tobacco and improving physical fitness. Wherever a law, regulation or ordinance has some impact on human health, it is the health department's job to promote, administer, or enforce it.
While their sheer variety may make these programs appear overwhelming, in practice they tend to sort themselves out rather tidily. The programs that protect health, as opposed to programs to promote it, have the virtue of being specific and concrete: licensing food handlers, for instance, involves testing for (or seeing the documentation of testing for) a finite set of conditions, and it becomes a simple pass/fail situation. Many of these programs can generate revenue for the local health department or reduce expenses for the local government. Most mandated licenses have a fee structure to cover their administration, and where the health department effort does not result in direct income it may perform services for other departments, saving money overall. Chronic disease control programs for the general public can, for instance, be woven into a city employee's wellness programs. The personal health services provided to city employees in an occupational health program and the savings to the city due to reduced sick leave and early return to work, thus improving overall productivity promote the health department's reputation and promote the case for additional resources at budget time.
The word "health" refers to the health and wellbeing of the entire community from its broadest aspects, their general physical fitness, mental health and nutrition, with an emphasis on early intervention to prevent onset of chronic conditions like hypertension and dental problems, to quite narrow attempts to modify deleterious behaviors, like smoking and drinking alcohol. Surprisingly, there were no objectives or goals for physical fitness in the first iteration of the Model Standards for Community Health Programs (Model Standards.) The 1990 Health Objectives for the Nation (1990 Objectives), however, provided several outcome objectives designed to get people involved in enjoyable activities that stimulate cardio-respiratory function and are appropriate to their ages. These were further modified in the Healthy People 2000, 2010, 2020 publications, which should be reviewed while reading this essay to compare the latest goals and objectives for each topic. They have since been modified further as seen in this PowerPoint slide set on Performance Standards from CDC's Office of Public Health Practice. Currently the prior “Model Standards” have been changed to the 10 essential services, in the above link to the National Public Health Performance Standards Program. The national program provides standards for
At the state level, the goal is often one of making a compelling case that fitness benefits the public. Texas collects a variety of data to measure effects of exercise on health costs, and school and job performance. The Virginia plan recognizes the responsibility of public health departments to work with other community agencies, profit and nonprofit, government and private to promote exercise and physical fitness. In the "Future of Public Health" this is the "assurance" function of the health department where the emphasis is on assisting other agencies to help the community, rather than expecting the health department to implement the services itself. The IOM’s 2003 publication on the Future of Public Health in the 21st Century, Chapter 2 focuses on “Understanding Population Health and Its Determinants”. Few local departments have specific objectives for exercise and fitness, though most can provide technical and research information on the value of these activities. The local health department is expected is to support groups interested in exercise while providing a balance between those who would emulate Mainland China by requiring everyone to perform public exercise, and the "couch potato". The data on the protective effects of exercise against heart disease are fairly good (Look at Framingham Data). Data on many other health benefits of exercise are not so well documented, often being little more than anecdotal accounts supplied by health activists. While promoting exercise is clearly a role for the public health department, a problem goal setters face is that the resources for exercise belong to private clubs, professional sports groups, recreation departments and sometimes employers. By working with YMCAs, recreation departments, athletic clubs, schools, colleges and sports minded groups to promote options for exercise and physical fitness, the heath department can lead its community, with small cost, toward better health. Physical fitness and its accompanying benefits provide a wonderful opportunity for role modeling by all public health staff. Unsuccessful health programs tend to lack a key ingredient; direct participation of their promoters. There is too much data on models and standards for any single agency to manage. It is the health director's and program manager's job to select the recommended standard appropriate for the community's current health status and resources available to enhance this health status.
Nutrition
The 2020 Recommended Objectivesfor Nutrition.
The first 15 objectives were retained from HP 2010, the remainder are new to HP 2020.
Even at the state level trying to meet all these goals with limited resources is problematic, at the local level it is necessary to take a more focused view. Besides setting general goals and promoting nutrition information, state and local programs usually aim to provide information on basic foods to segments of the population in need and, in the U.S., to actually provide special foods and food supplements to pregnant women, infants and young children. These programs are known as WIC programs. A detriment to focusing education on good nutrition to poor people is that these programs are managed by at least three different agencies. Pregnant women and infants found to have medical problems receive targeted food supplements from the WIC program, discussed later. Many of these same women are also eligible for food stamps, which they receive from social service departments. Poor school age children take part in school breakfast and lunch programs are managed by the Department of Agriculture. Some are also eligible for additional food through Community Action Programs. Lack of central coordination for these programs often makes them inefficient and vulnerable to abuse. Such abuse has been a major problem in many communities where the money vouchers intended for purchase of specific foods to combat medical problems, such as iron rich foods to combat iron deficiency anemia, are exchanged for cigarettes or alcohol, or even given to drug dealers to buy heroin!
Centralizing all food programs under the local health department or the local social services department may benefit the entire community. People suffering from poor nutrition can then receive medical intervention and nutritional counseling as well as food. Schools and public health departments, which often provide school nurses, can work together to focus on total nutritional education. Formal links can be developed between food purchasing, nutritional advice, health maintenance and treatment, and education using school children as change agents. There is an unexplored potential to change health status by linking the core curriculum for food and nutrition in kindergarten through 12th grade with food purchases in the various nutrition programs and the food provided at school meals.
A continuing major issue in the second decade of the 21st Century is that of childhood and adult obesity, although the definition seems to change almost daily it is clear that morbid obesity is associated with early mortality and much prior disability. Look again at the HP2010 and the HP2020 goals and objectives for nutrition to see how they have developed. Consider whether the objectives are clear, and whether they are likely to be met.
Fluoridation/dental health
Goal: Prevent and control oral and craniofacial diseases, conditions, and injuries and improve access to related services.
The above goal was the single HP2000 goal. In the HP2020 there are 17 objectives for Oral Health. Oral health is an essential and integral component of health throughout life. No one can be truly healthy unless he or she is free from the burden of oral and craniofacial diseases and conditions. Millions of people in the United States experience dental caries, periodontal diseases, and cleft lip and cleft palate, resulting in needless pain and suffering; difficulty in speaking, chewing, and swallowing; increased costs of care; loss of self-esteem; decreased economic productivity through lost work and school days; and, in extreme cases, death. Further, oral and pharyngeal cancers, which primarily affect adults over age 55 years, result in significant illnesses and disfigurement associated with treatment, substantial cost, and more than 8,000 deaths annually. Poor oral health and untreated oral diseases and conditions can have a significant impact on quality of life. Millions of people in the United States are at high risk for oral health problems because of underlying medical or handicapping conditions, ranging from very rare genetic diseases to more common chronic diseases such as arthritis and diabetes. Oral and facial pain affects a substantial proportion of the general population.
Fluoridation has been so successful that the Georgetown University School of Dentistry shut its doors in the early 1990s. Because of fluoride compounds in water, toothpastes and topical applications, along with the use of sealants for the dental enamel few children have serious dental problems any more. The major dental problem seen in many communities today is periodontal disease in older citizens.
Ideally, a single site dental program has one dentist, one dental hygienist, one dental assistant, and three operatories. The dentist provides acute dental care (with additional care for the elderly), while the hygienist applies topical fluoride and sealants. The hygienist may also give dental instruction in the school systems. Solo practitioner dental offices are still one of the few solo practitioner activities in the health care system.
High blood pressure.
The HP 2000 Objectives proposed: "at least 60 percent of the estimated population having definite high blood pressure (160/95 or greater) should have attained successful long term blood pressure control, i.e., a blood pressure at or below 140/90 for two or more years." This goal does not appear to consider the difficulty associated with changing the behavior of large numbers of people, particularly that of older people. Younger people, more likely to respond to education about lifestyle, will not experience health benefits from changes for 2030 years; this reduces the perception about the urgency of the message. The 2010 Objectives also link adverse behaviors (smoking, salt ingestion, overeating) with development of a community infrastructure to control them.
Review the HP2020 Objectives for hypertension control in the objectives for heart disease and stroke prevention
Change is best made gradually, at the local level, by helping communities adapt gradually to necessary changes that support their standards and beliefs. Attempts to impose changes in behavior by authoritarian approaches rarely work
In Virginia, with the emphasis by the State Board of Health on Chronic Disease, high blood pressure objectives are part of a chronic disease control program that ties health education and nutrition together. It focuses on risk factors related to lifestyle, all of which contribute significantly to the leading causes of death, such as:
Diet,
Smoking
high blood pressure
seat belt use
substance abuse
stress
exercise
use of weapons.
The 2014 biennial state budget for this program has been cut back significantly. It is very hard to explain the value of future health status based on public policy, where the policies are attached to fiscal statements for the budget period although it is probable as we collect better data with national level electronic health records it will be simpler to convince legislators about the value of preventing chronic disease rather than putting all your money into the acute diseases.
Dealing with chronic disease locally
Chronic disease programs must have public credibility for a local health department to carry them out successfully. In the 1980s Corpus Christi included chronic disease within its General Nursing program. All nurses were assigned to census tracts as well as clinics. Health educators worked closely with the nurses and clinicians to identify risk factors which they shared with organizations such as the United Way; cancer, diabetes, lung, and heart associations; the hospitals, doctors, nurses, dentists, pharmacists, and health clubs to show how people could change their behaviors, and improve their health. Each organization's board and volunteers examined the behavioral changes that fit into their long range plans. All agreed on the value of changes in nutrition, knowledge about blood pressure, reduced smoking, increased exercise and reduced stress. The local health department staff, without much fanfare, did what public health agencies do well: they developed consensus for health standards within the community. After 5 years, using formal reports that linked the major causes of death and disability with community changes needed to combat them, the media started paying attention to the annual reports and maps that showed who died where, and from what major causes. Also, maps that showed locations of deaths from traffic accidents, identifying those associated with alcohol. These actions raised the community's awareness about personal behaviors leading to illness, injury and death. Ongoing surveys, using population samples by income and geography, found that people felt they could change their behaviors to improve their health. The community's news media started to emphasize individual responsibility to avoid illness in news stories about new support groups for people with specific health problems, such as diabetes, Alzheimer's disease or cystic fibrosis. The media also gave publicity to statements by elected officials, which fostered community spirit among citizens to help one another avoid disease, disability and death. The Virginia Department of Health programs to reduce chronic diseases (updated in January 2015) and consider the diverse information and the shared agenda.
Despite the five or more years of effort needed to develop a community infrastructure devoted to health maintenance you should understand that it takes less in financial resources, than in leadership.
The role of the health department:
Smoking and health
The overwhelming majority of Americans believe that smoking affects health adversely. Besides proposing specific goals for the reduction of smoking the 2010 Overall Goal stated
Reduce illness, disability, and death related to tobacco use and exposure to secondhand smoke.
The objectives for adult tobacco use was:
Target and baseline:
Objective |
Reduction in Tobacco Use by Adults Aged 18 Years and Older |
1998 |
2020 |
Percent |
|||
27-1a. |
Cigarette smoking |
24 |
12 |
27-1b. |
Spit tobacco |
2.6 |
0.3 |
27-1c. |
Cigars |
2.5 |
0.2 |
|
|
|
|
Note that the 2000 Goal was utopian:
"by 2000 morbidity & mortality associated with tobacco use will be eliminated."
Not surprisingly, some southern states that are major tobacco producing states came to the table late with goals to eliminate tobacco use. While the existence of tobacco addiction and its relation to disease and death are supported by crystal clear data, public policy at the federal and state levels tended to be somewhat less clear until the late 1990s. The limited federal and state actions still leave room for an aggressive local health director to prevent additional disease, disability and death from a preventable cause. Local health departments exercised their unique working relationships with the cancer, lung and heart associations, and with the local restaurant associations, to develop strong clean air ordinances. They worked with coalitions to develop state and local ordinances to prohibit smoking in public places. Local ordinances have been developed in North Carolina and Virginia. In the 1990 session of the Virginia (the heartland of tobacco farming) legislature a statewide law against smoking in public places was passed with a specific prohibition against smoking in local health departments. Local departments kept the public informed about new research identifying and strengthening additional diseases caused by use of tobacco. They tried to influence insurance groups to offer lower rates to nonsmokers. In addition to the rising price of tobacco products themselves, the financial impact of related health problems can be a potent argument against smoking. Some local health departments tracked all smoking related deaths and morbidity reported by hospitals, nursing homes, funeral homes, and physicians; then analyzed the reports by age, sex and race to provide the news media with information useful to influence current smokers to stop smoking and children to avoid starting. Look at the Tobacco Use Control Project of the VDH to see how far the state has progress in recent years.
The 2020 objectives show how far we have come toward facing reality: Especially as local health departments nationally have lost 43.900 employees over the last period form 2008-2012 and are likely to face further cuts in the current deteriorating financial state systems. (Card see the NACCHO Report.)
Tobacco related Objectives for 2020 have been significantly amended:
Why Is Preventing Tobacco Use Important?
Tobacco use is the single most preventable cause of death and disease in the United States. Each year, approximately 443,000 Americans die from tobacco-related illnesses. For every person who dies from tobacco use, 20 more people suffer with at least 1 serious tobacco-related illness. In addition, tobacco use costs the U.S. $289 billion annually in direct medical expenses and lost productivity (CDC).
Healthy People 2020: A Framework for Ending the Tobacco Use Epidemic
Healthy People 2020 provides a framework for action to reduce tobacco use to the point that it is no longer a public health problem for the Nation. Research has identified a number of effective strategies that will contribute to ending the tobacco use epidemic. Based on more than 45 years of evidence, it is clear that the toll tobacco use takes on families and communities can be significantly reduced by:
- Fully funding tobacco control programs.
- Increasing the price of tobacco products.
- Enacting comprehensive smoke-free policies.
- Controlling access to tobacco products.
- Reducing tobacco advertising and promotion.
- Implementing anti-tobacco media campaigns.
- Encouraging and assisting tobacco users to quit.
The Healthy People 2020 Tobacco Use objectives are organized into 3 key areas:
- Tobacco Use Prevalence: Implementing policies to reduce tobacco use and initiation among youth and adults.
- Health System Changes: Adopting policies and strategies to increase access, affordability, and use of smoking cessation services and treatments.
- Social and Environmental Changes: Establishing policies to reduce exposure to secondhand smoke, increase the cost of tobacco, restrict tobacco advertising, and reduce illegal sales to minors.
The Abuse of alcohol and other drugs
A distinction is typically made between alcohol and other abused substances rather than using the term "abuse of alcohol and other drugs". Clearly, nicotine addiction, alcohol addiction, prescription drug addiction and illegal drug addiction share much common ground physiologically and behaviorally. From the behavioral point of view the only difference is the judicial danger associated with use of illegal drugs and the profit made from supplying them. Many local health departments do not have addiction programs since these have become the responsibility of the mental health, social services, corrections, and police and disabilities departments. The health department staff can find many examples of addiction on home visits and in occupational health programs. Employees who abuse alcohol and other drugs are generally referred to employee assistance programs. In such situations, the local health department's role becomes one of evaluating demographic, disease, disability and mortality data. Then it gives safety, police and social agencies outcome data to measure the effectiveness of their efforts. While the Virginia Department of Behavioral Health (VDBH, used to be the Virginia Department of Mental Health and Substance Abuse) and has specific substance abuse policies can you find a role within the VDH for such policies or for cooperation with the VDBH programs?
Control of stress and violent behavior
The HP 2000 and 2020 Objectives have changed significantly are now are found under the rubric of violence protection.
The healthy people 2020 goal and objectives are:
Violence Prevention
IVP-29 Reduce homicides
IVP-30 Reduce firearm-related deaths
IVP-31 Reduce nonfatal firearm-related injuries
IVP-32 Reduce nonfatal physical assault injuries
IVP-33 Reduce physical assaults
IVP-34 Reduce physical fighting among adolescents
IVP-35 Reduce bullying among adolescents
IVP-36 Reduce weapon carrying by adolescents on school property
IVP-37 Reduce child maltreatment deaths
IVP-38 Reduce nonfatal child maltreatment
Goal
Prevent unintentional injuries and violence, and reduce their consequences.
Overview
Injuries and violence are widespread in society. Both unintentional injuries and those caused by acts of violence are among the top 15 killers for Americans of all ages. 1 Many people accept them as “accidents,” “acts of fate,” or as “part of life.” However, most events resulting in injury, disability, or death are predictable and preventable. The Injury and Violence Prevention objectives for 2020 represent a broad range of issues which, if adequately addressed, will improve the health of the Nation.
Why Is Injury and Violence Prevention Important?
Injuries are the leading cause of death for Americans ages 1 to 44,1 and a leading cause of disability for all ages, regardless of sex, race/ethnicity, or socioeconomic status. More than 180,000 people die from injuries each year, and approximately 1 in 10 sustains a nonfatal injury serious enough to be treated in a hospital emergency department. 1
Beyond their immediate health consequences, injuries and violence have a significant impact on the well-being of Americans by contributing to:
- Premature death
- Disability
- Poor mental health
- High medical costs
- Lost productivity
The effects of injuries and violence extend beyond the injured person or victim of violence to family members, friends, coworkers, employers, and communities.
Understanding Injury and Violence Prevention
Numerous determinants (factors) can affect the risk of unintentional injury and violence.
Individual behaviors
The choices people make about individual behaviors, such as alcohol use or risk-taking, can increase injuries.3
Physical environment
The physical environment, both in the home and community, can affect the rate of injuries related to falls, fires and burns, road traffic injuries, drowning, and violence.4, 5
Access to Services
Access to health services, such as systems created for injury-related care, ranging from prehospital and acute care to rehabilitation, can reduce the consequences of injuries, including death and long-term disability.
Social Environment
The social environment has a notable influence on the risk for injury and violence through:
- Individual social experiences (for example, social norms, education, victimization history)
- Social relationships (for example, parental monitoring and supervision of youth, peer group associations, family interactions)
- Community environment (for example, cohesion in schools, neighborhoods, and communities)
- Societal-level factors (for example, cultural beliefs, attitudes, incentives and disincentives, laws and regulations)6
Interventions that address these social and physical factors have the potential to prevent unintentional injuries and violence. Efforts to prevent unintentional injury may focus on:
- Modifications of the environment
- Improvements in product safety
- Legislation and enforcement
- Education and behavior change
- Technology and engineering7
Efforts to prevent violence may focus on:
- Changing social norms about the acceptability of violence
Related Topic Areas
- Adolescent Health
- Maternal, Infant, and Child Health
- Mental Health and Mental Disorders
- Physical Activity
- Substance Abuse
By and itself Stress reduction is not an area where a health department can make changes primarily by its own efforts, as it does with immunizations. In some states this area is under the purview of departments of mental health; in others, it is related to abuse of alcohol, prescription and illegal drugs. Most of the hard data on the subject, however, are found in the medical examiner's files. Stress reduction, then, becomes another of the health department's functions identified in The Future of Public Health as an assurance function.
Health Protection
All the various programs designed to defend the public against hazards in their air, food, water and general environment come under the rubric of health protection. Many of these programs and associated goals have been part of public health since the Chadwick Report in the middle 1880s. They were similarly identified in England during the Cholera epidemic when Dr. Snow removed the handle of the community water supply pump near the Old Bailey, the Broad Street pump. Pollution of water by feces has long been known as a health hazard and its control was one of the first environmental movements. In developing countries provision of potable water has been a major contribution to reduced infant death rates. This has been particularly exemplified by the recent outbreaks of cholera in Haiti.
For at least 60 years major city and state health departments in the U.S. have placed a premium on clean and hygienic preparation, storage and serving of food to protect the public against diseases from typhoid, cholera, salmonella and hepatitis.
Since the Second World War there has been an increasing emphasis on protecting workers from harmful environments following studies of lung disease in mines and among shipyard workers exposed to asbestos. This has since been expanded to other chemicals in the factories and exposure to pesticides among farm workers. Since a record numbers of deaths in Donora, Pennsylvania in the mid-fifties during an atmospheric inversion, and the exposure to smog on the west coast, protection from air pollutants has had increasing emphasis.
Control of Toxic Agents.
The HP 2000 proposed a goal that
"the country shall achieve and maintain appropriate management of environmental pollutants so that morbidity and mortality associated with toxic substances will be reduced and adverse effects on the environment will be minimized".
This general goal statement is followed by objectives similar to those in the 1990 Objectives which set a blood lead level for young children and stated that
"By 2000 virtually no individual should suffer birth defects or miscarriage as a result of exposure to a toxic chemical, disposed after implementation of the Resource Conservation and Recovery Act."
The two major differences between the two documents are that the 1990 Objectives start each issue out with a general goal statement, followed by more specific objectives. The HP 2000 Objectives start out with a clear measurable objective. They are aimed at a national audience while the original ‘Standards’ were aimed at states and localities, and followed goals with objectives that were adaptable to communities, in most cases. They are models of objectives, not legally enforceable standards, despite the name.
By the time of publication of HP 2020 toxic substances protection is stated as follows:
Toxic Substances and Hazardous Wastes
The health effects of toxic substances and hazardous wastes are not yet fully understood.
Research to better understand how these exposures may impact health is ongoing. Meanwhile, efforts to reduce exposures continue. Reducing exposure to toxic substances and hazardous wastes is fundamental to environmental health.
A problem for health directors is that it is by no means certain just what a toxic substance is. Many claims of human health hazards from "toxic" exposures are based on tenuous data and extrapolation from animal studies. Of the more than 10,000,000 chemical compounds that exist fewer than 250 have had adequate population studies. The WHO’s International Agency for Cancer Research, located in France and globally recognized as the arbiter of carcinogenic standards, had classified less than just over 120 chemical compounds as carcinogenic. This agency also placed some 200+ into the two categories of 'possibly and probably carcinogenic.' See the section on evaluation of carcinogenic risks with attention to the preamble.
Much of our definitive knowledge about these compounds comes from industrial exposure studies. Little is known about the human effects of more than 64,000 additional chemicals used yearly in industrial processes, and until they have been studied, the arena will remain rife with political activism rather than science. The scientific basis for most of the new laws regulating known or suspected environmental hazards is also poor. Exposures to ALAR and EDBs, for instance, were unlikely to cause any harm to people, but the outcry against them was overwhelming. The purchase of apples declined so that a number of apple growers went out of business. Local residents in Triani, Alabama, claimed health problems from exposure to DDT, yet all that the Centers for Disease Control found in studies lasting several years was a difference of 2-3 mm. in systolic blood pressure. This may be a valid measurable statistical difference, but is certainly not a clinically significant one. The 1990 Objectives were set shortly after the Love Canal reports and reflected those concerns, yet long term studies of Love Canal residents have been able to link any excess disease or death to the exposures.
Since October 2001 there has been a resurgence of interest against attack by biologic agents. See the VDH role in these programs.
Local reassurance and explanation.
People in the USA today want guarantees that nothing can harm them; they want a risk free world. Because national public health professionals appear to have failed to respond adequately to these issues, city councils and county boards expect local health departments to reassure them about health hazards and explain why environmental control costs so much. Local health directors and their staffs must support local water companies and explain that costs of managing public water supplies are increased to protect them against chemical hazards, for which the evidence is often scanty. Until recently the only requirement was that water have sufficient chlorine at the end of the supply system to control salmonella bacteria. Now the water companies have to test more frequently for eight chemicals in addition to chlorine, and for biologic hazards in addition to salmonella. The chemicals include fluorides. Fluorides are naturally occurring constituents of water found in many areas of the country, particular in southeast Virginia. Although citizens have been drinking this water for centuries, with little effect other than brown stains on their teeth, the water company must reduce the level of fluoride below that which many dentists and physicians believe are necessary to protect health. The cost of fluoride removal may double or triple water bills for little or no benefit. Water companies are required to test water for lead. The lead, if found, is produced in the pipes of people's homes not by actions of the water companies. The water companies are expected to provide information to home owners, rather than the people who built, sold or rented the homes. Many local health departments have been testing children in homes suspected of exposing children to lead for years. Some local health departments have failed to find any evidence of lead among the community's children but they still have to work with the water companies, under the new laws, to assist in notifying people of these potential hazards, even if they don't exist!
As the result of laws passed in 1989 people have pay more for visits to doctor's offices to pay for protection from "medical wastes" which should cause little or no hazard. Although people produce waste they don't want their waste put in landfills in their communities, the NIMBY or "not in my back yard" syndrome. Health department staff must work with elected officials to explain that properly constructed waste disposal sites have little likelihood of causing harm to people or fauna. They have to be able to explain why an engineered site is better than allowing random dumping, which will occur in the absence of an engineered and permitted site. Local health departments must keep good records on causes of death by socioeconomic level and census tract or other geographic area and must be able to analyze distribution of death and disability to provide the community with an expert opinion about presumed environmental health hazards. The data must be good enough to demonstrate the clear existence of a hazard. Frequently, a local health director is asked to PROVE that some agent does NOT cause harm. It is not possible to prove that something does not cause harm, even if infrequently, only that it does. Such assertions are favorites for lawyers, investigative reporters and environmental activists. Avoid being trapped by semantics. Failure to avoid such a trap may make it impossible to present data derived by good research.
The health department is the health authority for the community, and its time is often wasted by discussion of environmental threats that may have nothing to do with its primary concerns. A chemical that is a threat to fish larvae is a matter for the local fish and game department, not the health department. The health department must confine itself to human concerns. Any other approach affects the credibility of the entire department.
Occupational Health & Safety
The 2020 Objectives list outcomes in terms of reduction in deaths, disabling injuries, lost workdays, skin and lung disease, hearing loss and heavy metal poisoning resulting from occupational hazards.
The original Standards proposed the goal that:
"Factors in occupational environments that cause, death, injury and disease or disability will be prevented or reduced; further personal damage from existing occupationally related illness will be minimized, and good health and well being among workers will be promoted."
In Texas in the 1980s the highest priority was the reduction of accidental deaths, disabling illness and injuries, and lost workdays by 10% by 1990, while in Virginia there was no reference to occupational illness and injury as these programs were found in the department of labor.
The following discussion from the HP 2020 healthy people objectives identifies more sophistication a national level on the issues of occupational health and safety:
Understanding Occupational Safety and Health
Work is one of the most important determinants of a person’s health. However, addressing occupational safety and health poses numerous challenges.
Related Topic Areas
![]() Educational and Community-Based Programs
Educational and Community-Based Programs
![]() Hearing and Other Sensory or Communication Disorders
Hearing and Other Sensory or Communication Disorders
![]() Respiratory Diseases
Respiratory Diseases
![]() Tobacco Use
Tobacco Use
![]() Vision
Vision
The workforce, like the U.S. population at large, is becoming increasingly diverse. These demographic changes result in new safety and health issues. For example, some workers—such as racial and ethnic minorities, recent immigrants, younger and older workers, workers with genetic susceptibility, and workers with disabilities—are more likely to have increased risks of work-related diseases and injuries. Workplaces are rapidly evolving as jobs in the current economy continue to shift from manufacturing to services. Major changes are also occurring in the way work is organized. Longer hours, compressed work weeks, shift work, reduced job security, and part-time and temporary work are realities of the modern workplace and are increasingly affecting the health and lives of workers.
Finally, the new chemicals, materials, processes, and equipment that are being developed at an ever-accelerating pace pose emerging risks to workers.
Despite these challenges, the Nation is poised to make significant improvements over the coming decade in the quality of life for all working people. Occupational safety and health research has led to many changes in workplaces and work processes that prevent injuries, illnesses, and deaths in workers. Ongoing research seeks to identify new and better ways to improve the health and safety of workers and to identify and address emerging hazards. In addition, scientists and partners are working together to translate and transfer research findings, technologies, and information into highly effective interventions and products that can be readily integrated into the workplace, resulting in more immediate improvements in the lives of workers.
Local programs
In some large cities and urban counties local health departments provide occupational health consultation and direction to the city/county manager, working closely with the personnel and safety departments.
In one city, for example, the program's goal is to:
"Optimize the health and safety of the city work force and minimize occupational illness and injury".
This was translated into managing a "wellness" program for all city employees and acting as occupational consultants to the city's school system. For 80% of its total cost of $189,920 the program provided a work force of approximately 3,600 persons with one occupational physician, one physician's assistant, one occupational health nurse and two clerks. The department recommended adding an additional occupational nurse to conduct the wellness programs and an industrial hygienist to monitor potentially hazardous exposures routinely, rather than waiting for the periodic examinations of hazards made by the city's insurance carrier.
Annual cost benefit studies showed that this program paid for itself. Its "early return to work program" offered counseling on the availability of light duty. The city's physician worked closely with the local physicians to make clear the availability of suitable light work for the city's employees, and the willingness of the occupational medical staff to monitor them for the treating physician. This was particularly important when employees were returned to physically hazardous programs in the public works and waste disposal areas. With a computerized database the staff was able to track city employees and record potential exposures of each one by employment site and activity and to conduct an epidemiologic study of back injuries. Data from this database led to supervision of employees who lifted heavy loads repeatedly; in both the public works and the sanitation departments.
Accident (unintentional injury) Prevention and Injury Control
The HP2000 specified lower fatality rates for automobiles, homes accidents such as falls, fires, scalds, drowning and firearm incidents, by mandating passive restraints for autos and smoke alarms for homes. The initialgoal was simply that "Mortality and morbidity associated with unintentional injury will be reduced."
In Virginia, accident prevention activities within several agencies were supervised by a prevention task force, chaired by the Secretary of Health and Human Resources. Many objectives encountered resistance and were unmet or changed. For instance, the public did not want automatic seat belts, though many were willing to use seat and shoulder belts once a state law made them mandatory. Prevention efforts aimed at drowning, falls, burns, childhood injuries and alcohol abuse were major initiatives of the departments of mental health and motor vehicles. The school system educated children to avoid injuries. The department of health ensured that emergency medical resources and a data tracking system was available.
In Healthy People 2020 the program recommends five areas important to injury prevention, found in the Overview Tab:
- The workforce, like the U.S. population at large, is becoming increasingly diverse. These demographic changes result in new safety and health issues. For example, some workers—such as racial and ethnic minorities, recent immigrants, younger and older workers, workers with genetic susceptibility, and workers with disabilities—are more likely to have increased risks of work-related diseases and injuries.
- Workplaces are rapidly evolving as jobs in the current economy continue to shift from manufacturing to services.
- Major changes are also occurring in the way work is organized. Longer hours, compressed work weeks, shift work, reduced job security, and part-time and temporary work are realities of the modern workplace and are increasingly affecting the health and lives of workers.
- Finally, the new chemicals, materials, processes, and equipment that are being developed at an ever-accelerating pace pose emerging risks to occupational health.
Emergency Medical Services (EMS).
In many cities, local health department staffs sit on emergency medical services advisory boards. With help from, and monitoring by, the state health department, these boards register emergency vehicles and set standards for those vehicles (including size, construction and contents) and for EMS staff training.
In some communities, for example, the board also included administrative and medical staff from major hospitals (a general and a children's hospital), the fire chief (who actually ran the system) and citizen members appointed by the city and county. The health department licensed and inspected all ambulances before they were put into service and annually thereafter, and the staff investigated all complaints and reported sanctions against providers (whether city or private) to the city council.
A local health director may receive complaints about response time. This can only be reduced if there is enough money to buy and strategically locate sufficient ambulances and crews to enable a response time of 10 minutes in many cities. Competition between agencies, particularly if one is private and one is public, is often difficult to resolve. Neither is potentially better than another, but local conditions may tip the balance. The best EMS programs are not just adjuncts to a fire or police department, but are supervised by persons with extensive training and experience, who have the authority and resources to manage them. Because EMS is often considered less glamorous than fire suppression and because more hazard pay is received for fighting fires than for attending to injuries, few firemen want to serve in an EMS position. The training for Advanced Life Support and Cardiac Technicians is extensive, and it is difficult to maintain such skills by rotating all firemen through the program for short periods. Thus private or separate emergency medical services may be preferable.
Disaster Preparedness
Each health department should have a disaster plan as part of its EMS program. The plan should designate disaster shelters and secondary emergency rooms to back up the community hospitals and should include provisions for staffing the hospitals with sufficient surgeons during crises. Either the major hospital's administrator or the health director should be made responsible to route patients from the disaster site to the hospitals. The plan should also show a source of additional vehicles for use as temporary ambulances and identify a temporary morgue, to be staffed by local funeral homes. Health department staff must be provided with passes to cross police barricades during such emergencies. Nurses can help staff additional emergency rooms and assist in evacuating people or visiting nursing homes after a disaster to ensure that there is enough food, water and power. The plan must prepare for an interruption of water supplies by outlining the ways potable water and waste disposal facilities can be provided by sanitary workers and by naming alternative water supplies. Annual disaster exercises test communications and all participants including police, fire department, civil defense, social services, mental health departments, public works, public utilities, hospitals, Red Cross and animal control services. The ability of health departments to respond to disasters has been enhanced by the Antiterrorism programs developed since October 2001. Virginia was recognized in 2009 as having one of the best Emergency Preparedness plans in the country, using an all hazards approach rather the just a biohazard approach, see the links to Agents & Threats and to Natural Disasters.
The Healthy People 2020 has a new section devoted to preparedness which provides the following goals and objectives:
Goal
Improve the Nation’s ability to prevent, prepare for, respond to, and recover from a major health incident.
Overview
Preparedness involves Government agencies, nongovernmental organizations, the private sector, communities, and individuals working together to improve the Nation’s ability to prevent, prepare for, respond to, and recover from a major health incident. The Healthy People 2020 objectives for preparedness are based on a set of national priorities articulated in the National Health Security Strategy of the United States of America (NHSS). The overarching goals of NHSS are to build community resilience and to strengthen and sustain health and emergency response systems.
To reach these goals, NHSS identifies the following objectives for urgent, focused attention:
- Foster informed, empowered individuals and communities. In
- Develop and maintain the workforce needed for national health security.
- Ensure situational awareness.
- Foster integrated, scalable health care delivery systems.
- Ensure timely and effective communications.
- Promote an effective countermeasure enterprise.
- Ensure prevention or mitigation of environmental and other emerging threats to health.
- Incorporate post incident health recovery into planning and response.
- Work with cross-border and global partners to enhance national, continental, and global health security.
- Ensure that all systems that support national health security are based on the best available science, evaluation, and quality improvement.
ENVIRONMENTAL PROGRAMS
Food protection
The 1990 Objectives were silent on this issue.
The original Model Standards proposed the goal that:
"the community will be protected against infectious and noninfectious foodborne illness," and an objective to measure the number of outbreaks associated with commercial establishments as an indicator of program effectiveness.
The HP 2010 document outlines a health code requiring inspections of restaurants and other food services and includes correction of deficiencies, identification of high risk foods, epidemiologic investigations when outbreaks occur, public information programs, instruction on personal hygiene in schools, and education programs for food service personnel. The code applies to institutional cafeterias in hospitals, schools, day care centers and jails, not just profit making restaurants.
For many years health departments wasted time performing physical examinations, fecal cultures, X-rays for tuberculosis or blood tests for syphilis as part of their food service programs. For the past two decades, the research has taught that foodborne illness is spread by a very few means: unwashed hands, improper cooking, improper storage, unclean utensils and contact between food and non food contact surfaces. Hopefully, no food service programs in the United States still require any of these personal tests as part of their food protection programs.
Model local health departments require all food services to have a certified food service manager on duty at all times. He or she must have passed a federally approved course of 16 hours of classroom instruction tested by written examination. The department must provide minimal classroom training (usually 24 hours) in basic food handling for all employees who come in direct contact with food. Qualified environmentalists who have passed federal standardization courses must inspect food service activities. Completion of these courses require that the student inspect the same place as the instructor under the same conditions, using the federal standardized reporting form, and that they arrive at the same conclusions within 5 percentage points of each other. Observation of food handlers at work discloses much about a food service operation, even before the sanitarian enters the kitchen. Those failing to wash their hands or keep their nails short and clean are likely to contaminate food. Such lapses are the responsibility of the certified food manager in charge. His certification can be removed, and he can be required to have further training. Look at the VDH registry of food service inspections and find out the status of your favorite eating place.
The healthy people 2020 goal and objectives for food safety states:
Overview
Foodborne illnesses are a burden on public health and contribute significantly to the cost of health care. A foodborne outbreak occurs when 2 or more cases of a similar illness result from eating the same food. In 2006, the Centers for Disease Control and Prevention (CDC) received reports of a total of 1,270 foodborne disease outbreaks, which resulted in 27,634 cases of illness and 11 deaths.
A foodborne outbreak indicates that something in the food safety system needs to be improved. The food safety system includes food:
- Production
- Processing
- Packing
- Distribution/Transportation 's
- Storage
- Preparation
Public health scientists investigate outbreaks to control them and to learn how to prevent similar outbreaks in the future. Success is measured in part through the reduction in outbreaks of foodborne illnesses.
Why Is Food Safety Important?
Foodborne illness is a preventable and underreported public health problem. It presents a major challenge to both general and at-risk populations. Each year, millions of illnesses in the United States can be attributed to contaminated foods. Children younger than age 4 have the highest incidence of laboratory-confirmed infections from:
- Campylobacter species
- Cryptosporidium species
- Salmonella species
- Shiga toxin-producing Escherichia coli O157
- Shigella species
- Yersinia species
Local cooperation
Long experience confirms that the food service industry is more willing to cooperate with local government regulations when it is allowed to take part in developing the regulations. For example; in 1980 in Corpus Christi, a resort area community, the restaurant industry was nearly at war with the health department, there were no standardized staff, the food protection program was minimal and the health department was still giving food handlers physical examinations. On the street, one of the main perceived values of the program was that prostitutes carrying a food handler's card were deemed safe from transmitting infection by both the police department and the general public!
A new director asked for a meeting of the local restaurant association. They were happy to have him on their "turf", listening to their problems. They did not believe physical examinations protected them from poor food practices. They wanted more frequent inspections. They actually wanted stronger enforcement, believing that a good reputation was vital for the tourist business. And, they most emphatically did not want the public to think that they only employed prostitutes or that everyone who carried a food handler's card was a prostitute. Listening to them revealed that there was no real cause for antagonism, their need for regulation coincided with the department's mandate to protect the public. It soon became clear that the restaurant association saw three particular benefits from a strong food code:
- Ease in knowing and keeping up with community standards
- Reduced likelihood of a foodborne outbreak hurting all their businesses; and
- Elimination of poor operators from the business.
Wanting to be part of the team, they formed a committee to consider such a code. An association member on the state restaurant board invited some owners of large restaurants with good reputations to join the committee. On the health department's side, the environmental supervisor asked outside sanitarians from health departments with excellent food service programs to visit the community and explain how their programs worked.
Together, the various groups revised the city code using models from other cities and recommendations from the USPHS and State Department of Health. The new code included; annual restaurant permit fees to cover the cost of training food handlers, provision for on the job training for food handlers; a requirement for a certified manager to be on duty during operating hours of all food service places; and a provision for food managers to supervise public food service programs at little league games, charity benefits, church suppers, etc., at no cost to the program or community, One year after the new codes became effective, the average inspection score increased 15 points to just over 90%. The health department agreed to teach sufficient courses in food handling so that public food events (very popular in South Texas) could be held without hazard to the community. After three years, more than 4000 persons had been trained as certified managers and more than 30,000 in a community of 300,000 trained as food handlers. This high proportion of the community trained in food handling testifies both to the high turnover in food service employees, the largest turnover in low paying industries, and to the large number of citizens involved in the voluntary food festivals, little leagues, and other public community events. Membership in the restaurant association increased, and the whole community became more interested in food hygiene.
What distinguished this community from others was the close working relationship between the health department and the food service industry. The health department was seen as an educator and quality controller rather than a bureaucracy. If a sanitarian found a certified manager performing poorly, the incident was discussed with the president of the food service advisory committee, who then called the offender. A public hearing was held to question whether the manager's certificate should be withdrawn. This was far more effective than going to court, food managers' performance, as measured by inspection scores, throughout the community rose rapidly after the first public hearing. Any suggestion of a food related incident resulted in rapid investigation by the department with a report to the advisory committee chairman.
The community's perception of the health department as a helping rather than controlling agency aided the department at budget time. Equal treatment for all providers, small and large, profit and nonprofit, was especially important. In second decade of the 21st century food service programs are based carrying out the FDA’s Hazard Analysis and Critical Control Point Principles and Application Guidelines (HACCP) Click on the links to principles and to retail & food services.
Waste water disposal
The original Standards set the goal that "residents of the community will not experience disease or adverse health effects from the substances associated with the management of waste water" in a consideration of waste water from the perspective of the individual homeowner's and the community's needs as well as ecological balance. As with food handling, the proposed outcome indicators reflect the number of disease outbreaks from handling, storing, transporting, disposing and recycling of wastewater. Few measurable effects on health result from malfunctioning home systems, but the failure of municipal and industrial systems is a serious matter indeed. The health director must interpret the impact of state and national standards set by bodies such as the Environmental Protection Agency on community services, and their costs. He needs to understand the process of treating waste water and the solids or sludge. This requires knowledge in toxicology, mutagenesis, cytogenesis, fetotoxicity and an understanding of risk assessment methods. The director must be adept at interpreting findings to the news media and to groups of citizens untrained in environmental science, also. These issues are discussed in another lecture
Septic system politics
Local health departments are usually responsible for ensuring proper waste disposal at individual home sites, issuing permits for sewage lagoons in rural areas, and approving disposal of treated septage on land. For the latter, the local health department serves as an intermediary between the applicant and a state agency, interpreting rules and regulations and indicating potential health hazards associated with such disposal. This is the most complex and most political operation in a local health department. The main difficulty with septic tank and drainfield installation is determining whether a proposed site has soil suitable for the installation. Rural areas with no central sewage system generally lack central potable water systems, too. A new landowner usually needs a way to dispose of wastewater along with a well for drinking water and rarely considers the likelihood of his septic tank contaminating his or his neighbor's fresh water. Different land formations have different drainage patterns. Where there are only four to six inches of topsoil over a layer of rocky substrate, for instance, a drain field may discharge 12" to 18" below the surface directly into shale. From there the effluent can drop rapidly (percolate) into an aquifer to pollute the ground water used for everyone's drinking. Realtors, landowners with major acreage, and contractors frequently sit on boards of supervisors and city councils. These individuals become upset when they cannot develop their land because of such drainage problems.
Explanation takes great tact and patience. Given the potential amounts of money involved, lawsuits over such matters are by no means unknown, and even if the department wins the law suit, the damage done to its community relations can be enormous. To avoid such wrangles, the health director and the department's environmental staff must educate city and county officials responsible for planning, zoning and issuing building permits about the problems caused by failing to check the septic system permit before issuing a building permit. They need to know that a percolation test alone rarely provides sufficient information on which to base issuance of an individual sewage system permit. Modern siting requires knowledge about soil profiles, water movement and retention in different soils, distance to water tables from the bottom of a septic system trench, amount of rock, sand or organic material in the soil and presence of aquifers or nearby surface water.
When the planning, water and sewage disposal departments review land available for building, considering where potential new developments are likely to be placed, they must consult with the health department to determine whether the land is suitable for individual septic systems or requires extension of central sewage systems. Soil scientists and certified civil engineers can plan, site and install individual home septic systems with general supervision by the health department's environmentalists. The environmentalists can spend their time on quality control by selecting sample installations to visit. First they check on the soil scientist's work by reviewing the soil profile report for the intended installation and observe a percolation test being performed. These observations are used to validate the selected drain field site in relation to the location and proposed home and well, if any. Following this they can review the engineering plans to be sure the engineer designed an appropriate sewage disposal system for the size of the home. The environmentalist will also need to observe sample sites to be sure the contractors install the systems according to the engineer's directions. Once the first few samples of either the soil scientist's or engineer's work have been found satisfactory fewer onsite inspections will be necessary to ensure good quality work.
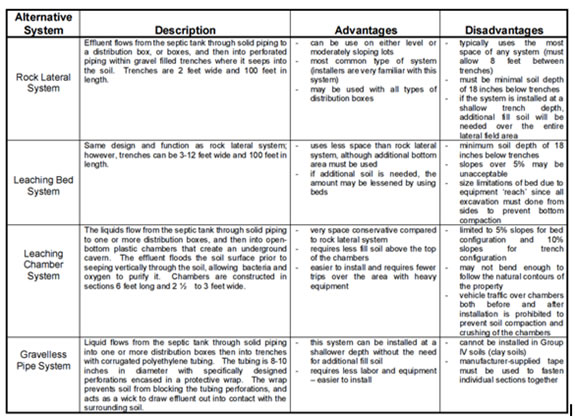
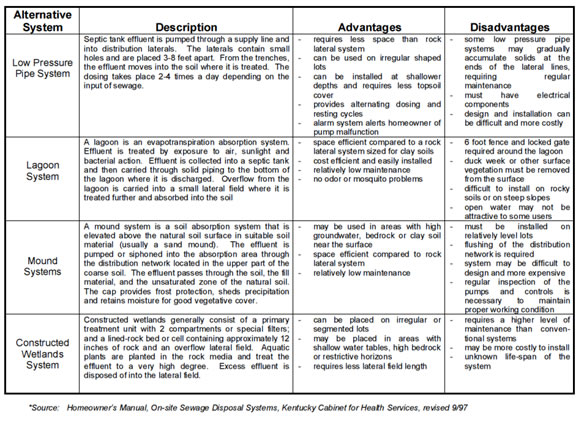
Increasingly as land to build on becomes scarce more innovation is needed to develop alternative liquid waste disposal systems, as shown in these two tables from the University of Kentucky monologue on waste disposal:
Polluted ground water
Health directors need assistance from epidemiologists, toxicologists, state biology and chemistry laboratories and state water resource staff to measure the effects of polluted aquifers on those who use them. When the aquifer supplies each home through its own well, each well owner has to deal with the problem individually. If the water is distributed through a public water system the water system owner is responsible for water quality. Unfortunately, in rural areas this is often an absentee owner living out of state and unresponsive to local actions. The problem may only be solved in court, and anything done there tends to cost a lot and take much time.
Meanwhile, the water users want instantaneous solutions. Before the polluting owner with a malfunctioning drain field or a business with faulty equipment can be placed under court order or disconnected, the health director is expected to be the expert keeping the public informed about potential ill effects. With many environmental activists ready to complain, but without authority to take action, the director has to develop strategies for education and crisis management in these situations. Another Lecture discusses crisis management in the health department.
Vector Control
The original Standards state that:
"Citizens should be at minimal risk of vector related diseases and conditions."
Goals for vector and animal control in the original Model Standards are identical to those in the 1990 Objectives, except for substitution of animal for vector.
HP2010 states: Vectors may be large farm or household animals but are commonly the insects found on these animals, in other words vectors are usually animals with exoskeleton (insects) as opposed to vertebrates. HP2020 no longer has a recommended objective for vector control, despite worldwide evidence of significant disease spread by insect vectors such as Ticks, mosquitoes and flies of various genera.
Animal control refers to actions taken mainly to prevent injury from animals rather than disease, with the exception of rabies. In the Model Standards animal and vector control are part of a single activity, yet the "animals" controlled by community animal and vector control programs are usually very different pets, on one hand, disease carrying insects, for the most part, on the other and the individual who does the controlling varies widely. The health department invariably deals with disease vectors. Animal control is a totally different function and should be separated from vector control. Unfortunately, when the original Community Model Standards and 1990 Objectives were developed they were developed generically at the national level, with little input from the few health departments that had responsibility for animal control. All have responsibility for vector control. Common vectors for diseases of public health importance are rats, bats, ticks and mosquitoes. Pigeons are often considered to be vectors by many members of the public who are concerned about the way they spoil public monuments by roosting and defecting. There is no evidence that pigeons are responsible for spreading any diseases to humans. A local health department should only be responsible for those creatures that become a public health problem by transmitting communicable diseases such as malaria, dengue, yellow fever, psittacosis and encephalitis, and not for those that are merely a nuisance, like pigeons and starlings.
Insect control
Vector control requires codes that reduce the insect population by reducing harborage for vectors and by destroying eggs, larvae or adults as necessary. Typically, such codes require inspection of backyards and industrial sites where waste such as tires and junked cars accumulate. To write good codes for the locality, it is essential to know the life cycle of the various insects living there: where they lay eggs, how long the eggs take to hatch, what kills or disables them or prevents reproduction, how far they fly and what attracts them. The Aedes mosquitoes, the vector for malaria, usually have a range measured only in hundreds of yards. The Culex quinquifasciatus, which are good biters and can spread encephalitis, can fly miles even in a strong wind. Each type of mosquito (there are over 1000 varieties in the U.S. alone) has its own behavioral characteristics. Luckily, only a few pose a disease hazard to man. Most vector control programs use as little insecticide as possible, focusing their efforts on harborage. Ditches and yards must be kept clear of stagnant water, trash and debris so that rain drains quickly into storm sewers. A glass of water or an empty can filled with rain water left outside the house for 10 days can brood an entire generation of mosquitoes. When on the wing, mosquitoes are best controlled with a micro droplet high intensity sprayer that disperses a very fine aerosol of Malathion some 50 to 100 feet. Because this spray cannot be seen, crews are often accused of driving through the community without doing anything, and some departments add a small amount of diesel oil simply to make the spray visible. Health departments in communities harboring disease carrying mosquitoes need to keep close surveillance for importation of malaria, dengue and yellow fever, encephalitis and West Nile virus. We must now worry about Chicungaya virus spreading from the Caribbean with the first case reported in Florida in January of 2015. In subtropical areas endemic typhus is a problem.
On the Gulf Coast a rash with fever is considered to be typhus unless proven otherwise. There, the frequent reservoir is the opossum, which cannot preen like other animals. It stands on a tree branch and shakes off the ticks, which may fall onto a passing pet, or later climb onto a pet that then brings the tick into the house. Like typhus and Rocky Mountain spotted fever, Lyme disease requires tick control. It is caused by a spirochete, Borellia burgdorferi, most prevalent in the northeast but found elsewhere. It is borne by ticks (commonly the Ixodes dammini, but also lone star and dog ticks). The host is often, but not always, a member of the mouse family. In one survey, 50% of impounded dogs, but no other pound animals, had antibodies against the Borellia. Lyme disease has been recognized with increasing frequency since 1980. It is important that physicians report occurrence of Lyme disease to health departments so they can advise citizens about protective measures.
Some state and local health departments take regular samples of ticks from animals known to harbor them. Others sweep fields and brush adjacent to woodlands where animals have been found with Lyme disease bearing ticks. These measures allow the local health department to warn the public about the potential for infection when they expose themselves to ticks. There is no way to eliminate ticks, but those going into areas inhabited by tick bearing animals can wear appropriate clothes, spray the clothing with tick repellant, check each other for ticks after potential exposure, and go to a physician for diagnosis and treatment if symptoms suggestive of Lyme disease or other tick borne disease occur within one to two weeks of exposure.
Rat control
Rats are controlled because they also carry diseases. They serve as hosts for vectors such as fleas, ticks and mites, which carry diseases such as typhus, plague and leptospirosis. Many authorities consider it unlikely that small mammals like rats and mice will survive with rabies and be a hazard to humans, but unlikely is not the same as impossible. Citizen requests to test any mammal for rabies needs to be taken seriously. The best way to control rats, whether roof or ground dwellers, is to reduce their harborage, food and water. Compliance with building codes minimizes roosts/nests for pigeons, rats and bats alike. Besides unprotected human food and garbage, rats eat pet food and water. Even if these are brought into the house, birdbaths and flowerpots can provide water. Even dog feces can support rats. It is often not easy to convince a pet owner that animal's wastes promote disease in this way. Codes requiring immediate gathering and disposal of animal wastes from streets and yards are essential for rat control. If rats have to be killed, it is advisable first to dust all their runways for fleas to reduce their escape when the rat nests are fumigated and dug up.
Bat control
Finally; a few words about bats, most are harmless and ecologically useful. The same building codes that protect homes from rats and pigeons, protect them from bats. While some insist that bats are not reservoirs of rabies, the local bat population should be sampled periodically for this disease (in Corpus Christi, for instance, 15% carry rabies). The vector control staff, in cooperation with the animal control section, can then use hard data in educating the community about bats. Because the rabies virus is present in the urine, saliva, and feces of infected bats people must be reminded repeatedly not to handle bats themselves or allow children or pets to play with dead, injured or ill bats. A live bat found lying on the ground is sick. A freeze in Corpus Christi killed several bats. A group of children found them and started playing with them, licking them, putting the heads in their mouths and throwing bats at each other. Because more than 10 children had played with more than 20 bats it was likely that one or more bats was rabid and one or more children infected. There was no way to identify which bat had come in contact with which child and in what way. It was important to know whether the child touched the bat, was covered with bat blood or urine, just touched the skin or whether the child had licked or mouthed the bat. All the children were immunized against rabies without, fortunately, having any reaction to the vaccine. In the last few years the major source of rabies among humans was bat bites.
Animal Control
In urban and dense suburban areas limited space increases the chance for contact between people and any free roaming animals that exist there. Pets frequently carry pests, contact stray (feral) animals, and can transmit at least 50 infectious diseases or infestations to their owners including rabies, Salmonellosis, tuberculosis, worm and amebic infestations, and all the tick and flea borne diseases. Dog feces, as noted earlier, attract rats, which live on their nutritional residuum. Pets can indeed be hazardous to our health. Dogs and cats are both territorial and will defend their homes. Male children are most likely to tease and be bitten by animals. There is more animal child contact when school is out, and animals are more likely to roam when the weather is good, so bites of boys peak in the summer. Both dog and cat bites can cause extensive tissue destruction, but dogs are generally larger and their bites can crush, and break bones while cat canine teeth will penetrate more deeply.
In some communities animal control is a police function; in others it is delegated to a humane organization, and in others the health department is responsible. In some communities the police or health department round up strays and gives tickets while the animals are boarded, by a local humane society many of which now operate strict no kill code programs for adoptions of the animals they board. Strict animal control is essential in urban areas not only to control stray animals but to reduce animal bites and the possibility of rabies transmission. Because there is a wide range in pet owners, from those who buy toy poodles as true pets to those who are antisocial and buy Doberman pinschers as guard dogs or pit bulls to fight other animals, animal control personnel need to be good judges of people as well as animals. The best workers dislike destroying animals of any kind and are good at public interaction, educating children and adults on the street and in classrooms. Their priority is to protect the public's health, not to issue citations. People are often much more protective of their pets than of their children, and animal control officers have been threatened, assaulted and shot at in the course of their work. They need the support of police and state game wardens. Keeping exotic animals such as snakes, ostriches, ocelots and even mountain lions, is a fad in some areas. Most people who own such animals do so to show off. After the glamour of ownership has worn off and the "pet" is no longer an infant and center of attraction, it is often abused. When the exotic pets reach puberty, their behavior changes and the cuddly animal may become dangerous. As none of these exotic animals can be immunized against rabies, they all pose a danger of carrying this disease, which has a long incubation period in most species. Such animals should be left in the wild. In the last 2-3 years many state legislative bodies have broadened the definition of animal control, dangerous animals, and owner responsibility.
Biting pets
Because of the increasing frequency of bites from animals running at large, many communities have increased animal code enforcement. Some codes allow only one non serious unprovoked bite before requiring an owner to show cause why the animal should not be either killed, or moved elsewhere. An individual whose pet has attacked people more than once can give the animal to someone in a rural area where the animal will not be a threat to the community. Law officers there are first told about the incident and given the opportunity to refuse relocation (which often happens). These codes state that when an animal bites twice, or once seriously, the owner must appear before the health director or judge for a public hearing. The bitten party, all witnesses to the incident, and lawyers are allowed to be present. The hearing is usually conducted by a hearing officer (often a city or county attorney). The health director has the option (by code) to kill, banish the animal from the community, or to require additional safeguards to keep it, with instructions to all concerned to report any violation. If rabies is prevalent in the community and the pet has not been immunized according to the law the animal can be killed and its head sent to a laboratory to be examined for rabies. Additional information on prevention of bites and the importance of preventing bites is found at websites at the CDC and the HSUS.
Animal control advisory boards
I cannot urge too strongly the appointment of an animal control advisory board for any health director who works with animals. Such a board provides an important link between the health department and a large segment of the community with common interests. Some kind of advisory board or community consultant should be developed for each major program area within the health department. This board reviews statistics on loose animals by type and location, and on bites by number and location. It acts as a public forum for people incensed about too many animals, failure of pickup of animals, behavior of animal owners and animal feces in the streets. The board reports periodically to the city/county council and discusses either loosening or tightening up laws, rules and regulations. It considers animal welfare and is concerned with prevention of unneeded animal/people contact, but also with acceptable behavior of pet owners, including the lodging and feeding of their animals. It can investigate animal abuse, develop standards for animal capture and disposal, and set conditions for the use of a capture loop or dart gun. The latter is used only when there is no danger to humans from shooting the gun, and the animal is likely to be rabid. The animal control advisory board acts as a buffer between the various elements of the community, the department and other governmental agencies, and the animals themselves. Just as important as dogs are cats which bite more frequently than dogs and are more likely to transmit rabies.
Housing Standards
The Model Standards state that:
"Residents will live in homes which are properly heated, cooled, clean and free from vectors, and have adequate space, light, water and sanitary facilities and proper food storage and preparation capabilities." In the latest iteration of healthy people, housing standards are no longer considered part of community health which is unfortunate and inappropriate. However, the APHA its publication National Healthy Housing Standard continues to define housing health as one of the major determinants of health, often not included in other such measurements and the surprise omission from HP 2020’
“Outcome measures” indicate incidence of childhood lead poisoning, accidents, fires, burns and presence of smoke alarms and fire extinguisher, while the “process measures” relate to presence of housing codes, inspection results, and follow up.
Few state health plans embrace housing programs, which are usually local. The local health department is ordinarily interested to see that housing codes are upheld to assure the health of inhabitants of low income rental housing. Building officials, using Housing Codes manage engineering and safety standards, not health standards. The housing standards of the American Public Health Association and the Building Code Officials of America (BOCA) emphasize health issues such as available potable water, adequate heating and cooling, available refrigeration to store food, and working toilets. These standards emphasize joint training of nurses and sanitarians to observe these standards and report substandard conditions to the building officials for enforcement if the health department is not responsible for code enforcement.
Experienced health directors confirm the value of having rental housing standards enforced by the health department. Rental housing standard programs require strong management, careful public education and, like other programs, should have their own advisory board. 60 years ago Portsmouth, Virginia, became a leader in ensuring availability of good quality rental housing for its lower income citizens. Prior to this time, because of illness associated with poor housing, the city council decided improvement of rental housing stock for the poor was a task for the health department and directed it to improve enforcement and reduce the prevalence of substandard housing. Since most of the problems were with rented, not owned homes, citations often resulted simply in poor tenants being evicted and left with nowhere to go. These houses were in terrible condition; all areas of the housing standards were being violated. Electrical systems were overloaded, lighting poor, lead based paint prevalent, water supplies absent, toilets nonfunctioning (often due to improper use by tenants), heating appliances unsafe and refrigeration lacking.
The temporary nature of tenant occupancy made it difficult to focus on individual complaints (rental units typically turned over every 15 to 18 months), and the department found that the ongoing block by block survey funded by a federal grant would take 20 years to complete. Homes were deteriorating faster than they could be brought up to standard. The housing advisory board was, to put it mildly, unhappy. The board of housing appeals, the health department's advisory board for the housing program, decided to focus on active surveillance of rental property and doubled the housing staff for this effort. Homeowners would be subject to passive surveillance. Neighbors, realtors, city staff on routine inspections, and public utilities would recommend owned homes for spot inspections. A new ordinance required that any rental unit from which the tenant moved could not be occupied again until it had been inspected by the health department and brought up to standard by the owner. If the owner refused, the unit would be condemned and sold or acquired by the city, subject to court action by the owner to prevent such action.
Each block in the community elected a block captain to report substandard housing to the health department. If the unit was occupied, every effort was made to find alternative housing for the tenant before citing the owner. The block captains in each neighborhood met quarterly with health department staff to discuss the quality of life in the neighborhood and ask the department, for example, to help clear weeds and debris. Where trash accumulations were a problem, the health department could cite the owner and require clearing by court order, this allowed contracting for the cleanup, and billing the owner directly.
Many of the public health nurses worked with families in the low income rental areas and could refer substandard housing to the environmental section for inspection and correction orders. The environmentalists, during a housing inspection, might see a potential problem requiring a nurse. Also, the community block captains would call either the nursing or environmental staff for help when needed.
This one program probably did more to weld nurses, environmentalists and residents into a team than any other in the department. As with other health department efforts, an effective public and media education program was necessary. As it became aware of the actual conditions and the efforts made to correct them, the public saw the department as equitably enforcing standards beneficial to the entire community. Over a three year period this program, alone, lowered the rate of substandard rental housing in the community from 46% to fewer than 3%.
Solid Waste Management
For all practical purposes this is a state function, as the EPA has delegated it to most states. Household and industrial wastes are usually deposited in controlled waste disposal sites designed to prevent decomposed products leaching into aquifers. These have clay bottoms and sides and nonporous liners. When the system is full, it is covered with a clay cap and vented to allow decomposition gases (mostly methane) to escape. Perimeter wells are placed around the site to monitor any leaching.
Municipal landfills used by cities and counties, mainly for household waste, are operated under a state license. Many are filling up because communities didn't make the long term and often expensive commitment to develop additional sites. Elected officials or citizen groups may call upon the health director to condemn landfill sites due to the Not In My Back Yard syndrome. As the official with the science and expertise, the director can work with local and state planners to find alternatives and help select the best one, and he can assure the people that waste is being properly dealt with.
Drinking Water
The Model Standards posit that,: "Residents will have access to drinking water that is free from harmful contaminants."
This should be a simple task given the recovery and purification technology of the 1990s. We can drill for ground water or treat surface water from lakes and rivers; we can use reverse osmosis to filter brackish or seawater; and we can filter water to remove cysts and kill the remaining microorganisms by contact with ultraviolet light, chlorine or bromine.
Yet, despite all this, in many rural areas there is little accessible potable water. Residents may place their wells too near drain fields and they may fail to grout the upper 50 feet of well casing properly to stop effluent and surface water from contaminating their wells. In U.S. urban areas the public water supplies meet state standards required by the EPA. The EPA adds additional standards almost annually and the states have to comply with them or lose the ability to set state standards. Until recently, the only test was to be sure there were no coliform organisms in the water. Now eight additional tests apply in all 50 states, and water costs more.
The EPA now requires that all public water supplies reduce their fluoride levels to 4 parts per million. In areas where fluoride levels are naturally high, private water supplies can easily exceed this standard. Other than tooth staining, there is no evidence that high fluoride affects health, but it is the health director's responsibility to tell the community why the federal standards are imposed so they can make informed decisions about how much they will spend to meet those standards and what the potential health and legal risks are for failure to do so.
In rural areas most houses are so dispersed that there is no cost effective way to provide public water supplies. Many small suppliers are stretched to their financial limit by current standards. In Virginia, estimates prior to the development of the recent EPA standards put the cost of providing drinking water, public and private, to everyone at more than $2 billion, a sum equal to the cost of Virginia's state and federal Medicaid funds together. A further $23 billion will be needed for wastewater treatment, and a like amount for solid waste disposal. This $2 billion is only for the 500,000 and more residents scattered across the countryside, not for the 6,500,000 already on the public water supply. The remaining $5 billion plus is to bring solid and liquid waste disposal systems up to current standards.
Communities are increasingly faced with water shortages from a combination of population growth and depleted aquifers and sometimes they have to ration water. This can mean no watering of gardens, except with heavily chlorinated sewage effluent, a shift from home laundries to group laundries. In some case, even, the health department may be called on to determine how long a person can retain reasonable hygiene without changing underclothes. After such calculation water restrictions can be tightened further. Reverse osmosis methods can be used to increase supplies when brackish water is available, but has not been used previously as a community wide resource in the U.S. In the mid 1980s small amounts of water were produced for the first time by reverse osmosis. Reverse osmosis has been used for some time in Israel. Trucking water is a very temporary solution. Water planning is rudimentary in most communities but will become more and more important with the continued increase of population.
Air Quality
This is usually a state concern because air crosses county and city boundaries. Like standards for water and solid waste, the EPA delegates air quality standards and enforcement to the states. Such delegation is known as primacy. The local health director, however, is the medical specialist who interprets pollution hazards to the public and local officials. He must describe acute and chronic effects and the different hazards of each type of pollution, and must stay informed about the community's health status. The department's staff should know which local industry has the largest smoke stacks, with the heaviest discharges and know what is emitted, how much, and how this affects overall air quality. The director should be knowledgeable about automobile and power plant contributions to air pollution and about passive smoking effects as well. People will have questions about their role in disability and death from such conditions as coronary heart disease, stroke, and chronic bronchitis, emphysema, and lung cancers.
Recommended Reading:
- Living Old. The Modern Realities of Aging in America. BS Video, Fall 2006
- Meeting the Challenge of Chronic Illness; Kane m, et al Johns Hopkins Press, 2005
- Guide to Community Preventive Services, Zaza S et Al, Oxford University Press, 2005.
- Beck A: The Ecology of Stray Dogs. Baltimore MD, York Press, 1972
- The 1990 Health Objectives for the Nation: Midcourse Review. US Dept. Of Health and Human Services, 1986.