2016
Chapter 9
Clinical programs
Wherever there is a significant population in poverty, without health insurance, or distant from medical facilities--or all three situations--the local health department should accept responsibility for ensuring access to a variety of programs to provide basic health and medical services. Most, but not all, of these services are directed toward infants and young children, who are seen not only as worthy objects of public support but also as a sensible investment of the public health dollar. It takes far less time and money to correct or eliminate a condition in childhood than it does to treat the later disability that the condition, if ignored, will produce.
The Institute of Medicine has encouraged enhanced funding of the National Health Service Corps (NHSC) scholarship program, to prevent a shift of family physicians away from rural communities, and to re-examine the role of local health departments and their access to primary care. Many local health departments already provide well child and prenatal care, family planning, home health care, immunization, STD services, follow-up care for chronic diseases, and other specialty services. It is relatively simple, in theory, to change from a system that focuses on clinics limited to treating federally funded conditions, the way most health department services are organized, to an integrated primary care system that focuses on people in family units. Internally, the greatest obstacle lies in redesigning the clinical database to secure an audit trail both to support federal and state funds and also to allow billing of third party payers. The director must enlist a wide base of support through partnerships. The most recent interest in coordination of clinical services, particularly in urban areas is known as a Health Care Safety Net (review the executive summary). This report although 10 years old has not been followed up by Congress or the AMA with any significant action but is recognized as valuable in the ACA which plans expansion of these programs. Before starting a primary care delivery program to ensure that all citizens have access to primary care, the director must search for the stakeholders among advisory boards of health professionals, elected officials and social agencies, as well as community activists to assist in developing a plan, to determine limitations, and whom the community’s future plan should cover. In rural and central city health departments’ primary care partnerships may be the wave of the future for delivering clinical public health services, particularly its new focus on chronic disease prevention. Take a look at this PowerPoint set from Sheryl Garland at VCU’s health care system about the central Richmond healthcare safety net as an example of community participation in delivering ambulatory care.
Primary care
The Original Model Standards proposed that:
"Residents of the community will have access primary health care services to promote achieving & maintaining optimal health status." It specifies that health departments shall "promote, encourage, and arrange primary care funding and service delivery from all appropriate providers. To the extent primary care services in the community are not adequate [the department] will provide such services directly or through purchase and cooperative agreements." The assurance function. The HP2010 objective is:
Increase the proportion of persons with a usual primary care provider.
Target: 85 percent.
Baseline: 77 percent of the population had a usual primary care provider in 1996
The HP2020 plan adds the following new Objectives for Health Access:
AHS-1 Increase the proportion of persons with health insurance and |
|
AHS-3 Increase the proportion of persons with a usual primary care provider is |
|
Which led to the following goals and analysis in the 2020 section on health access:
Improve access to comprehensive, quality health care services.
Access to comprehensive, quality health care services is important for the achievement of health equity and for increasing the quality of a healthy life for everyone. This topic area focuses on four components of access to care: coverage, services, timeliness, and workforce.
Access to health services means the timely use of personal health services to achieve the best health outcomes.1 It requires 3 distinct steps:
Disparities in access to health services affect individuals and society. Limited access to health care impacts people's ability to reach their full potential, negatively affecting their quality of life. Barriers to services include:
These barriers to accessing health services lead to:
Few states have developed long-range plans that include primary care, though many plans cite the need for citizens to have access to health care. Several states are revamping their indigent care programs to provide funds to reimburse hospitals and other providers for both institutional and primary care, as in Massachusetts, California and Oregon.
Many urban counties and cities as well as rural areas have large numbers of underserved, underinsured indigent populations for which the health departments provide primary care services (in Virginia in 2010 the percentage of the population without access to primary care was estimated to be 14%). Primary care has usually been delivered by agreements between the local medical society, the local community (tax supported) hospital and the health department. This is less costly than allowing people to wander into emergency rooms and usually has proven acceptable to the community. Primary care clinics (as opposed to private practices) are also an excellent way to bring adolescents into the health care system, to obtain their trust, and to help them understand and follow advice on healthy life styles. Health Departments might set school based health centers either on or next to high school campuses for maximum access.
In Portsmouth, Alexandria, and Newport News Virginia, the local health departments run the outpatient clinics of the community hospital. To make maximum use of limited resources and ensure that public health prevention programs, with their case management and health education components, did not lose visibility, they developed a system of general medical clinics, maternity clinics, pediatric clinics, and specialty clinics.
Tracking primary care programs
Data systems allow fiscal analysis of care and billing of third-party payers, whether the state's indigency fund (usually Medicaid), Medicare or occasionally, private insurance. Coding systems include CPT (current procedural terminology), ICHPPC codes (International Classification of Health Problems for Primary Care) developed by the North American Primary Care Research Group (known as NAPCRG) and DRG (Diagnostic Related Group) codes. Both the former codes were included to allow research that could compare both U.S. and international primary care research. Only CPT codes (currently CPT2000) are necessary for most U.S. primary care data systems. Data from surveys of the National Ambulatory Care Evaluation Survey (NAMCS) of the National Center for Health Statistics30 years ago show 24 common problems make up about half of primary care.
A study of the most recently available NAMCS survey (2012) shows little change in the prevalence of these conditions in family doctors’ offices in the last 30 years. The top twenty reasons to visit a primary care physician account for more than 50% of all visits. Ninety-five percent of primary care is directed at 150 different problems, most of which are fairly easy to treat. Increasingly, primary care also deals with life style issues, where changes may prevent certain diseases. Also look at the summary data tables from the 2012 survey, with particular attention to table 11 showing the 20 most common reasons for visiting a primary care physician.
These data satisfied auditing standards of state and federal programs, tracked public health programs and patients, and were used to ensure maximum efficiency, acceptability and availability to the clients. Because the clinic site in Portsmouth was near the hospital, the latter had access to patient charts when the clinics were closed--an ability to transfer records from the health department to the hospital is missing from most publicly supported primary care programs, one major reason for instituting electronic records systems. Access to the clinics was limited for some indigent patients due to lack of transportation. This became less of a problem as clients and transportation were linked together by timing clinics to start and finish in relation to available bus services, or to use transportation from other human service agencies to pick up and return patients, or in some cases to set up clinics in a facility near large numbers of patients. This model worked well for the development of the Hayes Willis Health Center in South Richmond 1992, as part of the health care safety net for central Virginia. The federal requirement that all medical care data be collected through Electronic Health Records Systems (EHRs) by the end of 2014 and incorporated into the ACA, should spur development of data systems that will allow fiscal, epidemiologic and quality analyses of medical care within the next 5 to 10 years, although probably not before 2020 instead of 2014.
As older primary care physicians have died or retired from practice they have been hard to replace. Nurse practitioners and physician’s assistants, when available, have been well received by patients, and the quality of care they provide has been excellent.
Genetic diseases
HP 2020 sets the following Goal and overview:
Improve health and prevent harm through valid and useful genomic tools in clinical and public health practices.
The new Genomics topic area and objectives for 2020 reflect the increasing scientific evidence supporting the health benefits of using genetic tests and family health history to guide clinical and public health interventions. This decade begins with recommendations from independent panels on genetic testing based on thorough reviews of scientific evidence.
The 1st recommendation is from the U.S. Preventive Services Task Force (USPSTF):
Women with certain high-risk family health history patterns for breast and ovarian cancer could benefit from receiving genetic counseling to learn about genetic testing for BRCA1/2. For women with BRCA1/2 mutations, surgery could potentially reduce the risk of breast and ovarian cancer by 85 percent or more.additional.
The 2nd recommendation is from the Evaluation of Genomic Applications in Practice and Prevention Working Group:
All people who are newly diagnosed with colorectal cancer should receive counseling and educational materials about genetic testing. Family members could benefit from knowing whether the colorectal cancer in their family is a hereditary form called Lynch syndrome.2 Screening interventions could potentially reduce the risk of colorectal cancer among men and women with Lynch syndrome by 60 percent.3
Genomics plays a role in 9 of the 10 leading causes of death, including:
Most states have genetic services in their maternal health programs that include testing for phenylketonuria (PKU), hypothyroidism, and sickle cell disease, among other genetic disorders. Positive test results are referred to the local health director who ensures that the affected child receives prompt final evaluation to decide the validity of the screening test. Depending on the genetic abnormality, special foods or counseling or both with be provided the parents. The local health department serves mainly to assure the availability and accessibility of these services. In the 2005 General Assembly, Virginia voted to increase testing from 17 conditions to 39. With the many current advances in genetic analyses coming on line we can expect more conditions to be covered, and hopefully more genetic screening and consultations prior to conception.
Laboratory services.
The outcome objectives are tests that include clinical microbiology (bacteriology, mycobacteriology, mycology, parasitology and clinical microscopy), virology, clinical chemistry, urinalyses, hematology, immunology, cytology, cytogenetics, blood banking and serology services. These laboratory tests support both clinical and environmental programs. For environmental health, ambient air analyses, water and wastewater analyses, analytic food chemistry, microbiology, clinical toxicology, virology, toxic substance analyses, and industrial hygiene testing are necessary to support services necessary to meet local, state and national objectives.
The local health department has to be concerned with quality as well as quantity of tests, and available manpower. Thus, the local health director must be concerned that specific tests can be performed only if there is sufficient demand for them and only by properly trained staff who meet all the standards required in federal regulations (42 CFR part 74) which have put all the laboratory quality standards required by Medicare and Medicaid into a single document. Many tests (such as HIV antibody or measles antibody) require special skills found only in large laboratories. The complexity of waste water effluent testing, as well as the increased range and limits of testing contents of ground water which requires such equipment as atomic absorption spectrophotometers and gas chromatographs limit this kind of testing to the largest commercial or state laboratories. Because of the concern for quality laboratory services only the largest city public health laboratories still perform clinical bacteriology in support of tuberculosis and Hansen's disease clinics. Due to increased screening for asymptomatic hypercholesterolemia, early onset of type-2 diabetes, and examination of children for Medicaid's early periodic screening, diagnosis and treatment programs (EPSDT) more local health departments are expanding their clinical testing using commercial equipment for which no standards have been developed. Before embarking on such endeavors the local director should ensure that he has a quality control program in place, supported by the state laboratory system.
Home care financial problems
Since the late 1970s most health departments in the U.S. eliminated their home health services due to competition from private profit making agencies. In Virginia for example, home health services started out as a state program to support social service agency clients. As home health service effectiveness became better understood, and as reimbursement was increased to move patients from hospitals and keep them out of nursing homes, a far more expensive placement for care, new profit-making agencies sprung up. However, "they skimmed the cream" by only taking care of paying patients, leaving the local health department in a "catch-22" situation. Many of those needing home health care were elderly or disabled people living on small fixed incomes, often without any insurance. Patients without insurance could not afford care from a private agency and looked to local health department home health care programs as a last resort, particularly in rural areas. The health department lost money delivering home health care to patients without ability to pay for care. Thus, the department first had to find out whether state or local government would be made up this loss, if not, it then had to decide whether to continue providing such services if the only alternative was to cut maternity or child health services or reduce immunizations. We can only hope that much of this lack of access can be cured as the "Affordable Care Act" matures.
Most local health departments find it impossible to compete effectively with private organizations. When income did not match expenses it was often because of a failure to ensure that all patients were enrolled in programs such as Medicaid, Medicare, TRICARE (the armed services third party payer system) or to take advantage of retirement programs offered by their employers. Because of superior case management programs, and the public health nurse's knowledge of the community, some local health departments are coordinating care between many different social and medical agencies to maximize benefits to patients. Private home health agencies usually provide only the specific technical service ordered by the doctor. Physicians who used services from both agencies have, mostly, preferred the case management approach provided by the local health departments. Home health services must have good data and financial systems. Many a good effort collapsed because a program extended itself further than its resources would stretch. As for other health department programs, audits are necessary to ensure accountability.
School health services
HP 2020 focuses on youth and adolescence:
Improve the healthy development, health, safety, and well-being of adolescents and young adults.
Adolescents (ages 10 to 19) and young adults (ages 20 to 24) make up 21 percent of the population of the United States.1 The behavioral patterns established during these developmental periods help determine young people's current health status and their risk for developing chronic diseases in adulthood.
Although adolescence and young adulthood are generally healthy times of life, several important public health and social problems either peak or start during these years. Examples include:
Because they are in developmental transition, adolescents and young adults are particularly sensitive to environmental—that is, contextual or surrounding—influences. Environmental factors, including family, peer group, school, neighborhood, policies, and societal cues, can both support or challenge young people’s health and well-being. Addressing the positive development of young people facilitates their adoption of healthy behaviors and helps to ensure a healthy and productive future adult population.
Adolescence is a critical transitional period that includes the biological changes of puberty and the need to negotiate key developmental tasks, such as increasing independence and normative experimentation. There are many examples of effective policies and programs that address adolescent health issues. They include:
The new approach in healthy people 2020 is to focus on the total environment which young children and adolescents develop, not just on school health.
Local health departments screen many children in the community from birth until school entry, to ensure that their growth is adequate, or if not that they receive expert attention. They also monitor the child's hearing, vision, and general health. Many poor children are followed either by the health department or private practitioners in compliance with Medicaid's EPSDT program. Some schools have excellent health services, most have none, a few are somewhere in the middle. The local health department's role in school health is often one of assuring the community that the services are effective, which it can best perform by seeing that HP 2020 goals are incorporated into the community's health service delivery system. Once children are admitted to school a school nurse should be available to work with the children's homeroom teachers to perform periodic screening of growth, vision and hearing, evaluation of weight in relation to height, and straightness of spine. The nurse has the responsibility to contact a child's parents when an evaluation shows an abnormality, and to make recommendations for referral.
The school nurse (in those communities that employ them) may be a public health nurse assigned to the school system by the local health department, using a memorandum of understanding, or may be a staff member of a school system that runs its own student health program. Just as in Virginia, the relationship of school health programs to the departments of education and health may be unclear. In some states the programs are assigned to departments of education, which obtain advice from local physicians. In others, the health departments provide them to the schools, using school premises to conduct the program, but setting the standards by agreement with the school systems. In most the issue is strictly a local issue and depends on whether the state or locality funds the program. There are a number of models for school health programs, but no consistent model has been developed across the country. This has occurred because schools have focused on educating children, and most health services are delivered to children by family doctors or pediatricians upon request of parents. It is only in the last decade that the medical profession, departments of public health, nursing associations, and parent's groups have started to unite to request standards of performance and state funding to meet those standards for school health services. This is probably the result of the increasing number of households with two working-parents and children getting sick when there are no medical services in schools. Another factor promoting increased school health services is the increased visibility of prevention and the link between prevention and education.
Process goals alone (e.g. Are children and staff exposed to programs?) do little to validate a program. Local health departments should have three aims for school health services:
Adolescents often find the school nurse one of the few persons they can trust to talk about problems of growth and development or about possible illness. Classroom teachers often ask school nurses to come to the classroom to provide additional information on health-related subjects, when the teacher does have enough knowledge. For both teachers and students the school nurse is an important authority on health matters.
Many school clinics are staffed with full time nurse practitioners and part time pediatricians or ephebiatricians (pediatricians who specialize in problems of adolescents). Comfortable waiting rooms and soundproof examining rooms to ensure confidentiality in the clinic help the staff to develop rapport with the students.
The local medical community, particularly pediatricians, has an important support role. Depending on the community's size, the pediatrician or family doctor has a major interest in children's health. With fluoridation of water supplies, and more recently application of sealants to enamel fissures, it is increasingly rare to see school children with cavities. The school dental programs supplement the activities of the privately practicing dentists by caring for children referred to them by the school nurse.
Family planning
Citing unintended pregnancy and infertility as both a personal and social burden, the 1990 Objectives called for:
"a reduction of unwanted pregnancies and of medications with a permanent effect upon fertility and for increased knowledge of contraception among the young."
The current data on unintended pregnancy and the live states visit the Guttmacher Inst. fact sheet for 2015.
Improve pregnancy planning and spacing, and prevent unintended Fregnancy.
Family planning is one of the 10 great public health achievements of the 20th century.1 The availability of family planning services allows individuals to achieve desired birth spacing and family size and contributes to improved health outcomes for infants, children, and women. 1
Family planning services include:
Abstinence from sexual activity is the only 100 percent effective way to avoid unintended pregnancy. For individuals who are sexually active, correct and consistent contraceptive use during every act of sexual intercourse is effective at preventing unintended pregnancy. Condom use is the only contraceptive method that protects against both unintended pregnancy and STIs; men and women should be encouraged to use condoms in addition to a long-acting, reversible contraceptive method at every act of sexual intercourse.
For many women, a family planning clinic is their entry point into the health care system and is considered to be their usual source of care. This is especially true for women with incomes below 100 percent of the poverty level, women who are uninsured, Hispanic women, and black women. Each year, publicly funded family planning services prevent 1.94 million unintended pregnancies, including 400,000 teen pregnancies.
These services are highly cost-effective, saving $4 for every $1 spent.
Unintended pregnancies are associated with many negative health and economic outcomes. Unintended pregnancies include pregnancies that are reported by women as being mistimed or unwanted. In 2001, almost half of all pregnancies in the United States were unintended. The rate of unintended pregnancies declined significantly between 1987 and 1994; however, since then, the rate has remained stable. The direct medical costs associated with unintended pregnancies in 2002 were $5 billion, or an average of $1,609 for each unintended pregnancy
Both Texas and Virginia set goals of reducing teenage pregnancies. Texas made education a priority: “all students in grades 4 through 12 will receive age appropriate education about reproductive health (including contraception instruction) in school on regular basis. In addition, at least 100 hours of quality prime time radio and TV announcements, commercials, and programs to improve reproductive health will be provided in Texas annually”.
Virginia, when developing its six year plans benefited from the Texas plan, the most recently developed, also from experiences at the national level and in other states, and relied heavily on local recommendations.
At the local level, in the city Corpus Christi and surrounding Nueces County, Texas, set as its goal:
"To ensure that each child born in Corpus Christi and Nueces County is a wanted child born to a mother able to care for that child."
The fertility rate in that county was 30% higher than the national average and significantly higher than other large urban communities with similar levels of indigence. Specific objectives included increasing the number of low-income fertile women coming to health department clinics by 33%, continuing Planned Parenthood services for children under 18 and improving data systems to help set better staffing ratios and perform general planning.
This program met 84% of the community's current needs and 60% of the needs identified in its long range plan. This required the supplemental staffing of 16 public health nurses, one health educator, six clerks and four community service aides. The original program cost $947,040 or 16.6% of the total departmental budget--an indication of the priority the department placed on the need for family planning services in the community.
When presented to the city and county managers, the plan was accompanied by a memorandum explaining that family planning services cost $87 per person per year versus at least $2,500 paid to the hospital district for each delivery, plus an additional $2,500 per year in support by the welfare department for each unplanned child. Ninety percent of those who dropped out of family planning programs became pregnant the following year. Seventy five percent of these become pregnant and were likely to have a high risk pregnancy if the program was cut. Between 20%-30% of the pregnancies of those denied family planning services had babies that were too small to survive unassisted, were delivered too soon, and consequently needed long term care in neonatal intensive care units costing $50,000-100,000 each. Data from state health department programs such as those in Virginia demonstrate that many infants surviving the neonatal intensive care units require support for developmental disabilities from schools and mental health programs.
Maternal and Child Health (MCH)
Like immunization, maternal and child health services are a basic health department program, available from many health departments since the beginning of the century. The 1990 Objectives set goals of lowered mortality rates for infants and pregnant women by racial group and region, also for a lower incidence of various congenital diseases/conditions of newborns. The Model Standards contain five pages of MCH objectives to reduce maternal and infant mortality. These will only be achieved by modifying national, state and local programs. These objectives contain three and a half pages of cross-references to the 1990 Objectives for MCH. The MCH objectives from the Model Standards also have four pages of references to objectives for school health programs and a further page of cross references to school health programs in the 1990 Objectives, all of which illustrate that national concern for children's health. Before proceeding further look at the HP2020 MCH Objectives.
Improve the health and well-being of women, infants, children, and families.
Improving the well-being of mothers, infants, and children is an important public health goal for the United States. Their well-being determines the health of the next generation and can help predict future public health challenges for families, communities, and the health care system. The objectives of the Maternal, Infant, and Child Health topic area address a wide range of conditions, health behaviors, and health systems indicators that affect the health, wellness, and quality of life of women, children, and families.
Pregnancy can provide an opportunity to identify existing health risks in women and to prevent future health problems for women and their children. These health risks may include:
The risk of maternal and infant mortality and pregnancy-related complications can be reduced by increasing access to quality preconception (before pregnancy) and interconceptional (between pregnancies) care. Moreover, healthy birth outcomes and early identification and t
reatment of health conditions among infants can prevent death or disability and enable children to reach their full potential
These objectives are helpful in providing some idea of the vast range of services and options for ensuring the health of mothers and children, the scope is so wide as to be impractical to cover for any local health departments. At the local level it is best to group several of these objectives together to make a single objective at the community level, for example it is possible to combine national concern for weight, hemoglobin levels, and meeting minimal vitamin intake into a single nutritional objective locally. Managers of local health departments must take the responsibility to examine the national models and select objectives that are applicable in their community. Each selection must be explained in clear and acceptable terms to the community otherwise the objectives may look like bureaucratic games. In a very few communities all the federal programs on nutrition from the MHC Bureau, Department of Agriculture and HHS have been integrated. However due to the technical oversight required by the various federal agencies this becomes extremely difficult. For further current information in Virginia, for example, look at this webpage on the core functions and essential services for maternal and child health programs throughout the state.
Statistical problems
Many of the initial model standards were not measurable or attainable on the basis of current knowledge and resources. The goal that
"no community should have mortality greater than 10% above the national level"
is useful. Locally, it may need to be restated as:
"No neighborhood/census tract should have infant mortality rate more than 10% above the community or state average".
In the healthy people 2020 document the whole issue of standardsand data management are grouped together under the public health infrastructure objectives and codified in the data and information systems:
PHI-7 (Developmental) Increase the proportion of population-based Healthy People 2020 objectives for which national data are available for all major population groups
PHI-8 Increase the proportion of Healthy People 2020 objectives that are tracked regularly at the national level
is it
PHI-9 (Developmental) Increase the proportion of Healthy People 2020 objectives for which national data are released within 1 year of the end of data collection
This lets the department focus resources where infant death rates are highest. When particular census tracts or neighborhoods do not have enough births or deaths to permit useful measurements, they can be aggregated into groups large enough to ensure that year to year trends and changes will be meaningful, not just deviations from the norm. Only meaningful changes can be related to changes in service. A census tract with about 100 births a year may have averaged one infant death a year for five years (a rate of 10 infant deaths per 1000 live births) but that five-year period could easily be composed of individual years ranging from 0 to 3 deaths per year (ranging between 0/1000 and 30/1000). Such chance fluctuations, resulting from small numbers, make the figures meaningless. It may be necessary to aggregate enough census tracts to measure a trend over the previous 5-10 years for comparison with the current year, and even this can be difficult for departments or communities with few births. In the last resort, surrogate indicators such as low birth weights or late attendance for first visit to prenatal clinic, can pinpoint need in the community.
State objectives
Both Texas and Virginia first followed the Model Standards and the "Healthy People" objectives in formulating their state goals for maternal and child health. Unfortunately, the Texas objectives were set just before the ‘oil bust’ that affected several gulf coast and mid-west oil states so badly, preventing planned increases in staff. In addition Texas has perennial high unemployment along the Rio Grande and a continual influx of Mexican and South American immigrants, problems that continue to strain its resources.
A time limit of six years was chosen for objectives in Virginia because there would be two years left in the current Governor's term, plus four years for the next Governor's term. Nothing planned further in the future would have any chance of political acceptance. The initial goals and objectives in Virginia were developed locally, where the services were actually given. The planning committee hoped this bottom-up approach would be more realistic and attainable.
Local objectives.
Over the short range the Corpus Christi, Texas, health department resolved to see more pregnant women earlier in their pregnancies. Specifically, they proposed an increase of 20% in their patient load of women at or below 150% of the poverty level, and a 15% increase (to 75%) of women entering the clinic by the end of their first trimester. The department decided that although many national objectives were useful, it would focus on two main measurable goals for a single year: these were: to increase total attendance at the maternity clinics, and
to reduce waiting time to enter clinics so that more women started maternity care during their first trimester of pregnancy. These objectives were easy to explain to the community and conformed to the state plan.
When the Corpus Christi health department developed its five-year maternity goals, the staff realized that they should define the local need, whether or not they were to be fully funded. This enabled them to budget for staff and decide strategies to meet the goals. Criteria used to develop these objectives included a total population of 300,000 people, no maternal deaths the preceding year, approximately 5,600 births, a fertility rate 32% higher than the state or nation, and 19,315 families with incomes less than the poverty level. Infant deaths in 1984 had risen to 65, compared to 54 in 1983 and 48 in 1982. Two of the pregnant women in the clinic during the year were only 12 years of age at time of delivery, which confirmed that the average age of conception was lower than for the state as a whole. Of the 74,479 fertile women in the county, 16.5% were at or below the poverty level and 28% were at or below 150% of the poverty level.
In Richmond VA, the health department found, as the result of a series of community wide focus groups, that too many citizens were falling through the gaps. In particular women attending MCH clinics has no resources when they had medical problems, other than going to emergency rooms. Over a period of ten years the local teaching hospital, the health department and local primary care physicians, banded together to develop an integrated community access system for primary care, a basic "health safety net". The clinics were moved from the health department to a new Primary care center, a community health center, to physicians' offices and to specialty clinics at the teaching hospital. During the development of the system it was found that 40 per cent of patients previously treated free had a source of payment for care. Many patients were being seen at several different sites and care duplicated. A pavement resource is developed if the patient does not have one. Care is coordinated. Cost has dropped significantly. ER room visits have dropped. The process was complex and supported by grants from the Robert Wood Johnson Foundation and by the Virginia Health Care Foundation. The role of the public health nurses has changed from clinical care to case management.
Malpractice problems
Increases in malpractice coverage premiums and in legal actions were reducing the number of physicians willing to deliver poor women. A perception by physicians that poor women were more likely to be at high risk and have adverse outcomes and that lawyers were more likely to talk these women into suing the delivering physician whether or not there was any real cause for action, underlay their reluctance.
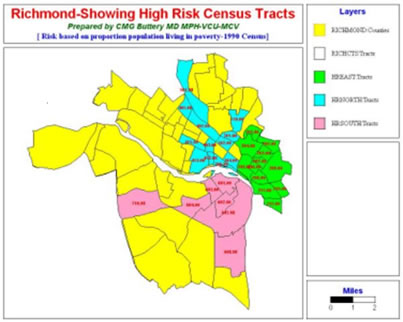
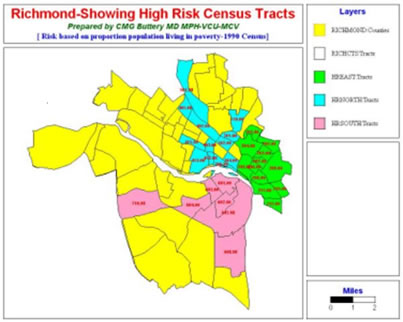
Data maps show the distribution of the economic groups and infant deaths in the community. Census tracts other than yellow are high risk.
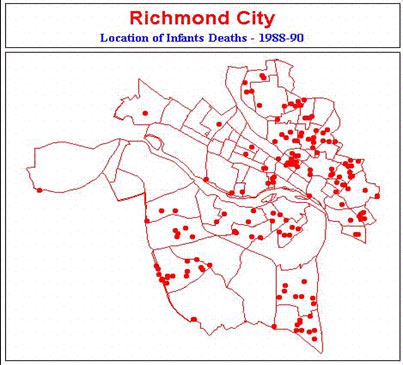
Poor women without adequate prenatal care are even more likely to have poor outcomes due to lack of good nutrition or abuse of tobacco, alcohol and other drugs. With several pockets of poverty in the city it would not have been surprising to see as many as 80 infant deaths per year, rather than 64. This leads to a liability problem for OB-Gyns. Rural states with sparse populations and distant major medical centers were hardest hit. This problem is described well in the Institute of Medicine's review of the effects of liability issues on maternity care (look at Summary & Conclusions). One potential solution being studied by many states is that taken by Virginia. The Virginia legislature developed a no-fault system for adjudicating damages to those infants neurologically damaged during birth. The definition of such damage was defined further during the 1990 legislative session. Analysis of its effect on lawsuits in 1998 showed that few claims had been filed, that those that were filed were legitimate and received compensation. The only concerns expressed were those of trial lawyers. Malpractice problems will continue to be a challenge but the newborn neurologically impaired infant law has halted the increase in premiums. Since the development of the neurologically damaged program liability rates stabilized the year of enactment and have dropped significantly over the last 10 years.
Seeking other alternatives
Local health departments are becoming the last line of defense against bad maternal outcome, and many departments are exploring alternative approaches such as contracting with local hospitals to deliver their patients. Under this plan, the local health department pays part of the salary of a hospital based obstetrician or nurse midwife, who then spends part of his or her time in the department's clinics and delivers the department's clients. In at least one state (North Carolina) rural physicians were coaxed into remaining in their communities when the state paid part of their liability insurance premiums in proportion to the number of health department or uninsured patients they deliver. Other local health departments contract for services with federally funded primary health care centers or migrant health care centers. Some states have provided funds to support primary practice directly. Others encourage physicians to stay in rural communities by providing continuing training and specialty-faculty support at nearby community hospitals through an area health education system (AHEC). Hopefully, a combination of these incentives, will not only ensure an adequate supply of primary care physicians, eventually, but will also help local health departments provide maternal and child health services.
State funding.
Some states have increased the funds available for maternal and child health by moving dollars from the general fund supporting the health department to the Medicaid program. This matches state with federal dollars, providing twice the funding otherwise available. This increase either permitted an increase in the eligibility level, for pregnant women and their children less than 12 years of age, from less than fifty percent of poverty to one hundred and fifty percent. Also this increase allowed reimbursement to be increased ensuring improved access to available services. In many states, the Medicaid reimbursement for maternity and other primary health care services was at or below 25 cents on the dollar of the actual cost to the physician or health department. Until the reimbursement, particularly in rural areas, was increased Medicaid coverage was of little value. By 1992 in Virginia Medicaid started paying more than Blue Cross. Physician acceptance of Medicaid enrollees increased quickly.
Staffing
As an example, four contract physicians, one nurse director, one nurse-midwife, one pediatric nurse practitioner, five nurse supervisors, 17 public health nurses, one community service aide, two and a half clinic aides, four clerks and one lab worker staffed the MCH program in Corpus Christi. These people were distributed over eight sites at various times of the week. To meet the department's long term goal of providing care to all women below 150% of poverty and their children, additional staff of a second nurse-midwife, ten public health nurses, two nutritionists, one community service aide, one clinic aide and two clerks would have been needed.
Since a single program covering both maternity and child health makes effective use of a small staff, it did not make administrative sense to separates these services. The same nurses provided care to both, making home visits to mothers and children in the same household. Nurses were assigned to care for patients in specific census tracts and staffed the clinic sites that covered those census tracts. In the community there were 86,934 children under 18 years of age. Of this number, the state regional handicapped/developmental disability program served 442. The local department looked after another 108. Of the 8,474 Aid to Families with Dependent Children (AFDC) recipients in the county, 5,739 were children. From this analysis of potential workload, the following objectives were set for the next year:
The Corpus Christi health department, like 99% of its peers, was understaffed; yet felt it was their responsibility to ensure that all citizens received care even if it was not possible to deliver this care within the department. Toward this end, the department developed links to residency training programs at two of the three general hospitals in the city and with the nursing staff at two smaller county hospitals. The nursing supervisory staff and health director were on the medical or nursing staff of the community hospitals where they taught preventive medicine, worked out plans for community coverage of emergencies affecting health department clients, and kept the health care-personnel in the community knowledgeable about the department's capacities and limitations. This resulted in full support by the health care community for the department's efforts.
Case managers
It is possible to train individuals in each agency to act as ombudsmen or "case managers" to help clients through the government agency maze. Once efficiency is placed second to effectiveness, clients can be served with relative ease by multiple agencies. Few institutions are as complicated as hospitals. One hospital in Japan set a standard that any service requested should be available within 60 seconds. In Virginia it is now possible to go to a Department of Motor Vehicles office anywhere in the state and get a new license, or a registration renewed, within two minutes, on most days, and within seconds on the internet. Similar goals should be possible for human services. The health department's multiple programs lend themselves to electronic linkage to track performance data. Health agencies can and should be leaders of effective and efficient government programs. In 2009 in Virginia (and most states) linkage between social and health programs with a move to case management systems is still an untested future, despite a 15 year demonstration of its effectiveness in Arlington County, Virginia
Budgeting and garnering support
When budgeting to meet the objectives discussed above, the Corpus Christi health department decided to state the danger of reducing--rather than the benefit of increasing--resources. Any reduction would increase not only infant deaths but also the number of developmentally disabled children requiring additional mental health, education and social support services. The cost of these additional services would by far exceed the prenatal care cost of $700 each per year for the additional women. A grant of $100,000 had become available from the Texas state health department for early identification of women at high risk, who could be referred early in their pregnancy to the community hospital for evaluation and specialized care. The staff calculated the expected increase in infant deaths and handicapped children per 1000 births that did not occur because of this $100,000 grant, based on trend data, and used these projections to justify additional staff. The department also used data comparing the cost of neonatal intensive care units with the several hundred thousand dollars worth of community services to care for a child with cerebral palsy (as a representative developmental/birth injury outcome) through 18 years of age. Had the costs been extrapolated for life, even though this might be less than the average life span for developmentally disabled children the costs of care would increase even further as the current guardians became older and unable to care for the child.
Local health departments must look for financial help from many sources: state, special federal projects, local government, United Way and other health care organizations. Some private foundations such as W.K. Kellogg or Robert Wood Johnson foundations provide grants for certain goals that are reflected in health department programs. The alert health director works closely with Community Action Programs, community and migrant health centers, free clinics, local hospitals, residency programs, and allied health training programs to plan services to avoid duplication. Moreover the director will not ignore the possibilities of revenue from Medicaid, state funded hospitalization programs, local welfare, and even private insurance.
Women, Infant and Children's (WIC) nutrition programs.
In a typical urban health department the WIC program absorbs 6% of the total budget. The program goal is to
"identify pregnant and nursing women, infants and preschool children at nutritional risk and provide supplementary food."
Corpus Christi had a potential of 12,000 pregnant women and young children at nutritional risk each month (those living below 150% of poverty). Thirty-four percent were served each month through the use of funds provided by the state, all but two percent of those certified eligible receiving service. This service was integrated into the maternal and child health program because it was so intimately related to the MCH clients. This is the pattern for most local health departments. One of the best outcomes is that WIC programs have encouraged an increasing number of pregnant women to enter MCH programs as soon as they become pregnant, to receive the food benefits. Thus, WIC serves as a portal to the public health system for many who otherwise might never have come to the prenatal clinics.
Research has provided little evidence that children who enter WIC programs are significantly different from children who go to health department prenatal clinics without a WIC program. Most evaluations have been directed at the question of whether the mother learned how to answer questions after each nutrition session, not whether she actually changed her diet. It may not be a good assumption that being able to answer questions correctly means that nutrition changes.
Tracking mothers and children
The WIC program requires accurate counts of patients and of families (or households) served, as well as all relevant medical information on them. A complete record of the treatment provided and the outcomes is the basis for a statistical measure of program effectiveness and efficiency; from this, the likely results of care can be estimated with some precision. It is also valuable to track the department's cost to deliver care. Comparing this cost with that of a private system, public hospitals or other providers such as primary care centers indicates whether WIC services are cost effective and cost efficient, or whether it would be cheaper to contract with other providers. Different communities use different options.
Promote health and reduce chronic disease risk through the consumption of healthful diets and achievement and maintenance of healthy body weights.
The Nutrition and Weight Status objectives for Healthy People 2020 reflect strong science supporting the health benefits of eating a healthful diet and maintaining a healthy body weight. The objectives also emphasize that efforts to change diet and weight should address individual behaviors, as well as the policies and environments that support these behaviors in settings such as schools, worksites, health care organizations, and communities.
The goal of promoting healthful diets and healthy weight encompasses increasing household food security and eliminating hunger.
Americans with a healthful diet:
All Americans should avoid unhealthy weight gain, and those whose weight is too high may also need to lose weight.
Diet and body weight are related to health status. Good nutrition is important to the growth and development of children. A healthful diet also helps Americans reduce their risks for many health conditions, including:
Linking maternity, family planning and child health programs in a central data system insures proper follow-up after delivery of an infant, and the connection with the community's vital data system permits a direct evaluation of outcomes. With complete data, it is possible to compare outcomes for patients in the program with those who go to private physicians, or who get no care. Data on how many maternity clients and their children use the WIC program and whether birth weights differed depending on their use of these special nutrition programs have medical value. The data system is optimal if it permits referral of children to any school lunch and breakfast program. The linkage for such an integrated public health data system is described in more detail in the chapter on data systems.
Recommended Reading: